Sunday Poster Session
Category: Biliary/Pancreas
P0192 - A Case of Acute Biliary Obstruction Due to Severe Hemorrhagic Pancreatitis and Duodenitis Due to Riluzole
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed K. Osman, MD, MPH
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Mohamed K.. Osman, MD, MPH1, Ahmed Shaikheldin, MD2, Matthew A. Kalloo, MD2, Diahann Seaman, MD2, Joan A.. Culpepper-Morgan, MD, FACG3
1NYC Health + Hospitals/Harlem, New York, NY; 2Harlem Hospital Center, New York, NY; 3NYC Health + Hospitals, New York, NY
Introduction: Riluzole is a new therapy for amyotrophic lateral sclerosis (ALS). Gastrointestinal side effects are reported in 5-10% of patients. Recurrent pancreatitis has been reported. Our patient presents unusually with severe hemorrhagic pancreatitis, leading to biliary obstruction.
Case Description/
Methods: A 74-year oldfemale with ESRD, recent arterial stent, and ALS presented with 4 days of abdominal pain. ALS was diagnosed 4 months ago. PEG tube placed one month later. Riluzole was started 2 months prior to admission. Her pain was periumbilical, 10/10 in severity, intermittent, and associated with vomiting. WBC was 11.62 x103/mcl, Hb 16.9 g/dl, and platelets 203. BUN 91, creatinine 9.7, and calcium 11.5. Albumin was 4.4, total bilirubin 1.3, direct bilirubin 0.4, alk phos 107, ALT 18, and AST 57. Lipase was 1004. She was given IV fluids and opioids for acute pancreatitis. CT scan showed a 3.6 cm peripherally enhancing fluid collection in the wall of the descending duodenum, resulting in dilation of the common and pancreatic ducts. In the first and second duodenum, there was wall thickening, submucosal edema, and adjacent fat stranding. The common duct measured 7 mm. The gallbladder contained high-density material with enhancement of the cystic duct wall. The main pancreatic duct was 4 mm. Apixaban and clopidogrel were held. Antibiotics and high dose PPI were started. EGD revealed no ulcers. It showed an intact gastrostomy tube and a large ampulla. Biopsy was non-diagnostic. One day later her anemia worsened. Hb went to 9.7, WBC 6.28, and platelets 55 from baseline. Lipase improved to 89 U/L. BUN/ creatinine increased to 94/ 10.9. CT abdomen angiogram confirmed the duodenal wall fluid collection obstructing the ampulla. Endoscopic ultrasound (EUS) showed spontaneous oozing of blood and pus from the large duodenal bulge. After the EUS there was marked decompression. However, she continued to bleed and eventually underwent successful gastroduodenal artery embolization. Her riluzole was discontinued indefinitely. She continued on dialysis and desmopressin for uremic coagulopathy. Her abdominal pain resolved and her Hb remained stable at 7.9 g/dl. Her clopidogrel and apixaban were resumed.
Discussion: The introduction of riluzole 2 months prior to the diagnosis, pointed to the medication as a culprit, as has been reported in a similar case. IV fluids and discontinuing the medication are the mainstay of management. Uremia and anticoagulant therapy likely contributed to the severity of the bleeding.
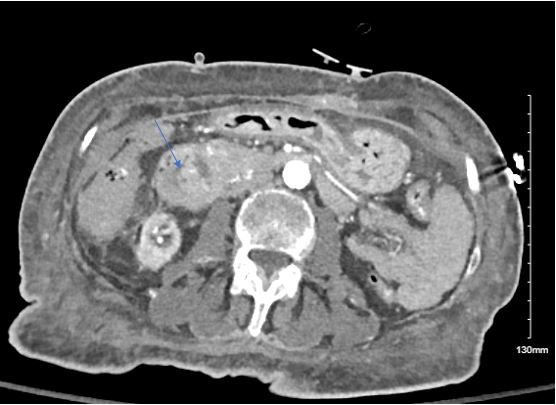
Figure: Duodenal thickening

Figure: Second portion of Duodenum
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Ahmed Shaikheldin indicated no relevant financial relationships.
Matthew Kalloo indicated no relevant financial relationships.
Diahann Seaman indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH1, Ahmed Shaikheldin, MD2, Matthew A. Kalloo, MD2, Diahann Seaman, MD2, Joan A.. Culpepper-Morgan, MD, FACG3. P0192 - A Case of Acute Biliary Obstruction Due to Severe Hemorrhagic Pancreatitis and Duodenitis Due to Riluzole, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Harlem, New York, NY; 2Harlem Hospital Center, New York, NY; 3NYC Health + Hospitals, New York, NY
Introduction: Riluzole is a new therapy for amyotrophic lateral sclerosis (ALS). Gastrointestinal side effects are reported in 5-10% of patients. Recurrent pancreatitis has been reported. Our patient presents unusually with severe hemorrhagic pancreatitis, leading to biliary obstruction.
Case Description/
Methods: A 74-year oldfemale with ESRD, recent arterial stent, and ALS presented with 4 days of abdominal pain. ALS was diagnosed 4 months ago. PEG tube placed one month later. Riluzole was started 2 months prior to admission. Her pain was periumbilical, 10/10 in severity, intermittent, and associated with vomiting. WBC was 11.62 x103/mcl, Hb 16.9 g/dl, and platelets 203. BUN 91, creatinine 9.7, and calcium 11.5. Albumin was 4.4, total bilirubin 1.3, direct bilirubin 0.4, alk phos 107, ALT 18, and AST 57. Lipase was 1004. She was given IV fluids and opioids for acute pancreatitis. CT scan showed a 3.6 cm peripherally enhancing fluid collection in the wall of the descending duodenum, resulting in dilation of the common and pancreatic ducts. In the first and second duodenum, there was wall thickening, submucosal edema, and adjacent fat stranding. The common duct measured 7 mm. The gallbladder contained high-density material with enhancement of the cystic duct wall. The main pancreatic duct was 4 mm. Apixaban and clopidogrel were held. Antibiotics and high dose PPI were started. EGD revealed no ulcers. It showed an intact gastrostomy tube and a large ampulla. Biopsy was non-diagnostic. One day later her anemia worsened. Hb went to 9.7, WBC 6.28, and platelets 55 from baseline. Lipase improved to 89 U/L. BUN/ creatinine increased to 94/ 10.9. CT abdomen angiogram confirmed the duodenal wall fluid collection obstructing the ampulla. Endoscopic ultrasound (EUS) showed spontaneous oozing of blood and pus from the large duodenal bulge. After the EUS there was marked decompression. However, she continued to bleed and eventually underwent successful gastroduodenal artery embolization. Her riluzole was discontinued indefinitely. She continued on dialysis and desmopressin for uremic coagulopathy. Her abdominal pain resolved and her Hb remained stable at 7.9 g/dl. Her clopidogrel and apixaban were resumed.
Discussion: The introduction of riluzole 2 months prior to the diagnosis, pointed to the medication as a culprit, as has been reported in a similar case. IV fluids and discontinuing the medication are the mainstay of management. Uremia and anticoagulant therapy likely contributed to the severity of the bleeding.
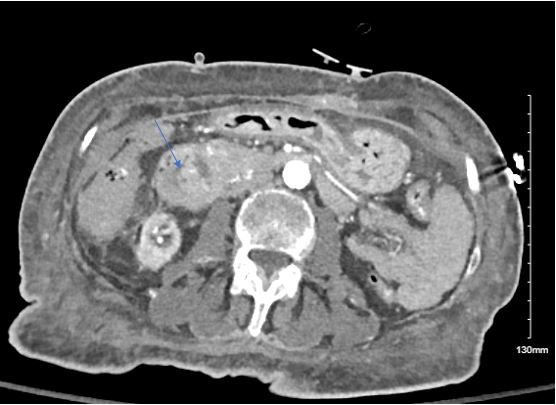
Figure: Duodenal thickening

Figure: Second portion of Duodenum
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Ahmed Shaikheldin indicated no relevant financial relationships.
Matthew Kalloo indicated no relevant financial relationships.
Diahann Seaman indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH1, Ahmed Shaikheldin, MD2, Matthew A. Kalloo, MD2, Diahann Seaman, MD2, Joan A.. Culpepper-Morgan, MD, FACG3. P0192 - A Case of Acute Biliary Obstruction Due to Severe Hemorrhagic Pancreatitis and Duodenitis Due to Riluzole, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
