Sunday Poster Session
Category: Biliary/Pancreas
P0185 - When Doxycycline Took a Detour: An Unlikely Cause of Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JM
Jasjit Multani, MD (he/him/his)
Unity Health-White County Medical Center
Searcy, AR
Presenting Author(s)
Jasjit Multani, MD, Kelley Ingram, DO, Katherine Treacy, DO
Unity Health-White County Medical Center, Searcy, AR
Introduction: Drug-induced pancreatitis (DIP) is responsible for up to 2% of all acute pancreatitis (AP) diagnoses. We present the case of an elderly male with acute DIP likely due to doxycycline administration.
Case Description/
Methods: A 73-year-old man presented to his outpatient primary care provider’s office with concerns of productive cough and he was prescribed a 7-day course of doxycycline 100 mg twice daily for treatment of suspected pneumonia. After 2 days of doxycycline administration, the patient presented to the emergency department in moderate distress with sudden-onset 10/10 squeezing epigastric pain with radiation to his back and associated nausea and vomiting. Lipase resulted at 8739 units/L. CT of the abdomen and pelvis with IV contrast showed diffuse pancreatic edematous changes with prominent peripancreatic fat stranding. He was administered intravenous fluid resuscitation, intravenous opioid analgesics, and intravenous antiemetics. Doxycycline was discontinued and he was transitioned to azithromycin for 3 days. His symptoms improved and he began tolerating oral intake on day 2 of hospitalization. Repeat lipase level on day 3 revealed significant improvement to 33 units/L. The patient was transitioned to regular diet which was tolerated well. He remained symptom-free on day 4 of admission and was discharged with close follow up.
Discussion: Even though many medications cause DIP, our case underscores the importance of recognizing doxycycline as a rare cause of DIP. In this case, the patient developed classic symptoms of acute pancreatitis—sudden, severe epigastric pain radiating to the back—shortly after initiating doxycycline. Laboratory evaluation revealed a significantly elevated lipase and imaging confirmed pancreatitis. Other common causes such as alcohol use, gallstones, and hyperlipidemia were excluded. Early discontinuation of doxycycline with initiation of supportive care led to rapid improvement and normalization of pancreatic enzymes. The temporal association, absence of alternative causes, and resolution after drug cessation strongly support a diagnosis of DIP. Clinicians should maintain awareness of this rare but serious adverse effect. In patients presenting with acute pancreatitis of unclear etiology, a thorough medication review is essential. Early recognition of potential drug-related causes can guide prompt management and avoid unnecessary diagnostic interventions. Further studies are needed to understand the mechanisms by which doxycycline causes DIP.

Figure: Figure 1 - CT of abdomen and pelvis with IV contrast with the transverse view of the pancreas
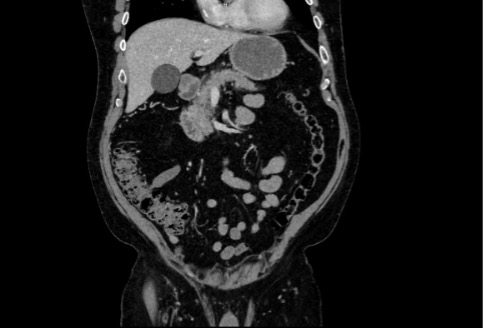
Figure: Figure 2 - CT of abdomen and pelvis with IV contrast with anterior/posterior view of the pancreas
Disclosures:
Jasjit Multani indicated no relevant financial relationships.
Kelley Ingram indicated no relevant financial relationships.
Katherine Treacy indicated no relevant financial relationships.
Jasjit Multani, MD, Kelley Ingram, DO, Katherine Treacy, DO. P0185 - When Doxycycline Took a Detour: An Unlikely Cause of Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Unity Health-White County Medical Center, Searcy, AR
Introduction: Drug-induced pancreatitis (DIP) is responsible for up to 2% of all acute pancreatitis (AP) diagnoses. We present the case of an elderly male with acute DIP likely due to doxycycline administration.
Case Description/
Methods: A 73-year-old man presented to his outpatient primary care provider’s office with concerns of productive cough and he was prescribed a 7-day course of doxycycline 100 mg twice daily for treatment of suspected pneumonia. After 2 days of doxycycline administration, the patient presented to the emergency department in moderate distress with sudden-onset 10/10 squeezing epigastric pain with radiation to his back and associated nausea and vomiting. Lipase resulted at 8739 units/L. CT of the abdomen and pelvis with IV contrast showed diffuse pancreatic edematous changes with prominent peripancreatic fat stranding. He was administered intravenous fluid resuscitation, intravenous opioid analgesics, and intravenous antiemetics. Doxycycline was discontinued and he was transitioned to azithromycin for 3 days. His symptoms improved and he began tolerating oral intake on day 2 of hospitalization. Repeat lipase level on day 3 revealed significant improvement to 33 units/L. The patient was transitioned to regular diet which was tolerated well. He remained symptom-free on day 4 of admission and was discharged with close follow up.
Discussion: Even though many medications cause DIP, our case underscores the importance of recognizing doxycycline as a rare cause of DIP. In this case, the patient developed classic symptoms of acute pancreatitis—sudden, severe epigastric pain radiating to the back—shortly after initiating doxycycline. Laboratory evaluation revealed a significantly elevated lipase and imaging confirmed pancreatitis. Other common causes such as alcohol use, gallstones, and hyperlipidemia were excluded. Early discontinuation of doxycycline with initiation of supportive care led to rapid improvement and normalization of pancreatic enzymes. The temporal association, absence of alternative causes, and resolution after drug cessation strongly support a diagnosis of DIP. Clinicians should maintain awareness of this rare but serious adverse effect. In patients presenting with acute pancreatitis of unclear etiology, a thorough medication review is essential. Early recognition of potential drug-related causes can guide prompt management and avoid unnecessary diagnostic interventions. Further studies are needed to understand the mechanisms by which doxycycline causes DIP.

Figure: Figure 1 - CT of abdomen and pelvis with IV contrast with the transverse view of the pancreas
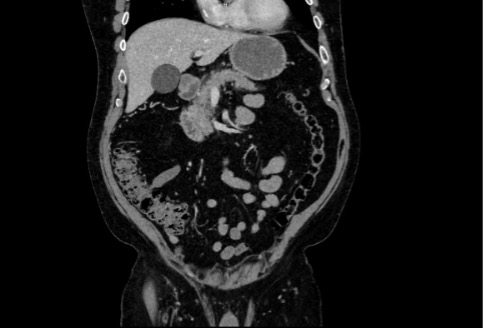
Figure: Figure 2 - CT of abdomen and pelvis with IV contrast with anterior/posterior view of the pancreas
Disclosures:
Jasjit Multani indicated no relevant financial relationships.
Kelley Ingram indicated no relevant financial relationships.
Katherine Treacy indicated no relevant financial relationships.
Jasjit Multani, MD, Kelley Ingram, DO, Katherine Treacy, DO. P0185 - When Doxycycline Took a Detour: An Unlikely Cause of Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
