Sunday Poster Session
Category: Biliary/Pancreas
P0178 - A Rapid Descent: Early Walled-Off Necrosis and Hepatic Infarction in Acute Alcoholic Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Simran Rameshbhai Patel, MD
Bayhealth Medical Center
Dover, DE
Presenting Author(s)
Simran Rameshbhai Patel, MD, Ayesha Jamil, MD, Syed Mahmood, MD, Abhishek Agnihotri, MD
Bayhealth Medical Center, Dover, DE
Introduction: Acute pancreatitis (AP), often due to alcohol or gallstones, ranges from mild to severe necrotizing form. We present a rare case of early walled-off necrosis (WON) and hepatic infarction. In this young patient with chronic alcohol use, AP quickly progressed from typical symptoms to a severe, life-threatening illness.
Case Description/
Methods: A 38-year-old man with chronic alcoholism presented with acute epigastric pain, nausea, and vomiting. Labs revealed leukocytosis, thrombocytopenia, AKI, elevated lipase ( >4000 U/L), and AST/ALT (2173/255 U/L). CT confirmed AP without necrosis. He progressed to septic shock, ARDS, hypoxia induced PEA arrest, and anuric ATN requiring renal replacement therapy (RRT). Repeat imaging showed necrotizing pancreatitis, splenic vein thrombosis, and a right hepatic infarct. The patient continued to improve and was successfully extubated and discharged.
Discussion: AP can lead to peripancreatic fluid collections that evolve into pseudocysts or WON, typically after 4 weeks. WON results from inflammation or direct injury to the pancreatic duct, causing extravasation of pancreatic fluid and enzymes into the parenchyma. Vikesh Singh et al. found that up to 27% of patients had early walled-off collections within 3 weeks. In alcohol-induced AP, WON is noted to develop in approximately 10–15% of all cases, and in up to 30–40% of those with necrotizing pancreatitis.
Moreover, hepatic infarction is extremely rare due to the liver's dual blood supply and usually reflects focal vascular occlusion or severe localized ischemia. SIRS-induced hypotension or DIC may promote microvascular thrombosis and segmental liver necrosis. Portosplenomesenteric venous thrombosis is found in up to 50% of patients with necrotizing pancreatitis. It may result from the local extension of inflammation or pseudocyst-related vascular erosion. Also, IL-6 mediated systemic inflammation and WBC activation may lead to hepatic vascular endothelial injury by releasing elastase and reactive oxygen species, increasing the risk of infarction.
This case emphasizes the importance of maintaining a high index of suspicion for atypical complications in AP. Early and comprehensive imaging, particularly with contrast-enhanced CT, is essential for the timely identification of evolving complications such as WON and hepatic infarction. Clinicians should be alert to signs of systemic deterioration or vascular compromise, which may herald the onset of these severe complications.
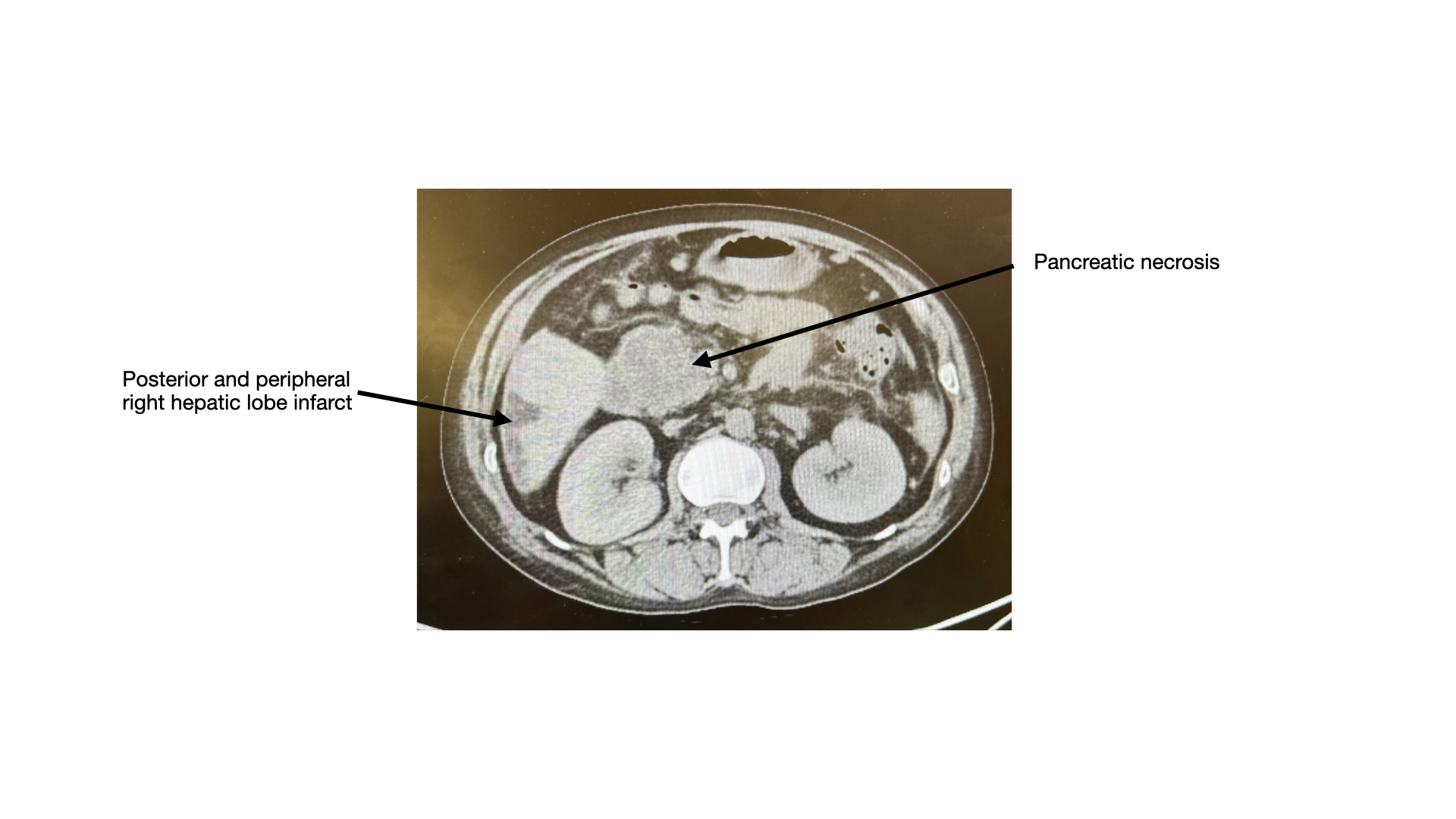
Figure: CT Abdomen and Pelvis without contrast
Disclosures:
Simran Rameshbhai Patel indicated no relevant financial relationships.
Ayesha Jamil indicated no relevant financial relationships.
Syed Mahmood indicated no relevant financial relationships.
Abhishek Agnihotri indicated no relevant financial relationships.
Simran Rameshbhai Patel, MD, Ayesha Jamil, MD, Syed Mahmood, MD, Abhishek Agnihotri, MD. P0178 - A Rapid Descent: Early Walled-Off Necrosis and Hepatic Infarction in Acute Alcoholic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Bayhealth Medical Center, Dover, DE
Introduction: Acute pancreatitis (AP), often due to alcohol or gallstones, ranges from mild to severe necrotizing form. We present a rare case of early walled-off necrosis (WON) and hepatic infarction. In this young patient with chronic alcohol use, AP quickly progressed from typical symptoms to a severe, life-threatening illness.
Case Description/
Methods: A 38-year-old man with chronic alcoholism presented with acute epigastric pain, nausea, and vomiting. Labs revealed leukocytosis, thrombocytopenia, AKI, elevated lipase ( >4000 U/L), and AST/ALT (2173/255 U/L). CT confirmed AP without necrosis. He progressed to septic shock, ARDS, hypoxia induced PEA arrest, and anuric ATN requiring renal replacement therapy (RRT). Repeat imaging showed necrotizing pancreatitis, splenic vein thrombosis, and a right hepatic infarct. The patient continued to improve and was successfully extubated and discharged.
Discussion: AP can lead to peripancreatic fluid collections that evolve into pseudocysts or WON, typically after 4 weeks. WON results from inflammation or direct injury to the pancreatic duct, causing extravasation of pancreatic fluid and enzymes into the parenchyma. Vikesh Singh et al. found that up to 27% of patients had early walled-off collections within 3 weeks. In alcohol-induced AP, WON is noted to develop in approximately 10–15% of all cases, and in up to 30–40% of those with necrotizing pancreatitis.
Moreover, hepatic infarction is extremely rare due to the liver's dual blood supply and usually reflects focal vascular occlusion or severe localized ischemia. SIRS-induced hypotension or DIC may promote microvascular thrombosis and segmental liver necrosis. Portosplenomesenteric venous thrombosis is found in up to 50% of patients with necrotizing pancreatitis. It may result from the local extension of inflammation or pseudocyst-related vascular erosion. Also, IL-6 mediated systemic inflammation and WBC activation may lead to hepatic vascular endothelial injury by releasing elastase and reactive oxygen species, increasing the risk of infarction.
This case emphasizes the importance of maintaining a high index of suspicion for atypical complications in AP. Early and comprehensive imaging, particularly with contrast-enhanced CT, is essential for the timely identification of evolving complications such as WON and hepatic infarction. Clinicians should be alert to signs of systemic deterioration or vascular compromise, which may herald the onset of these severe complications.
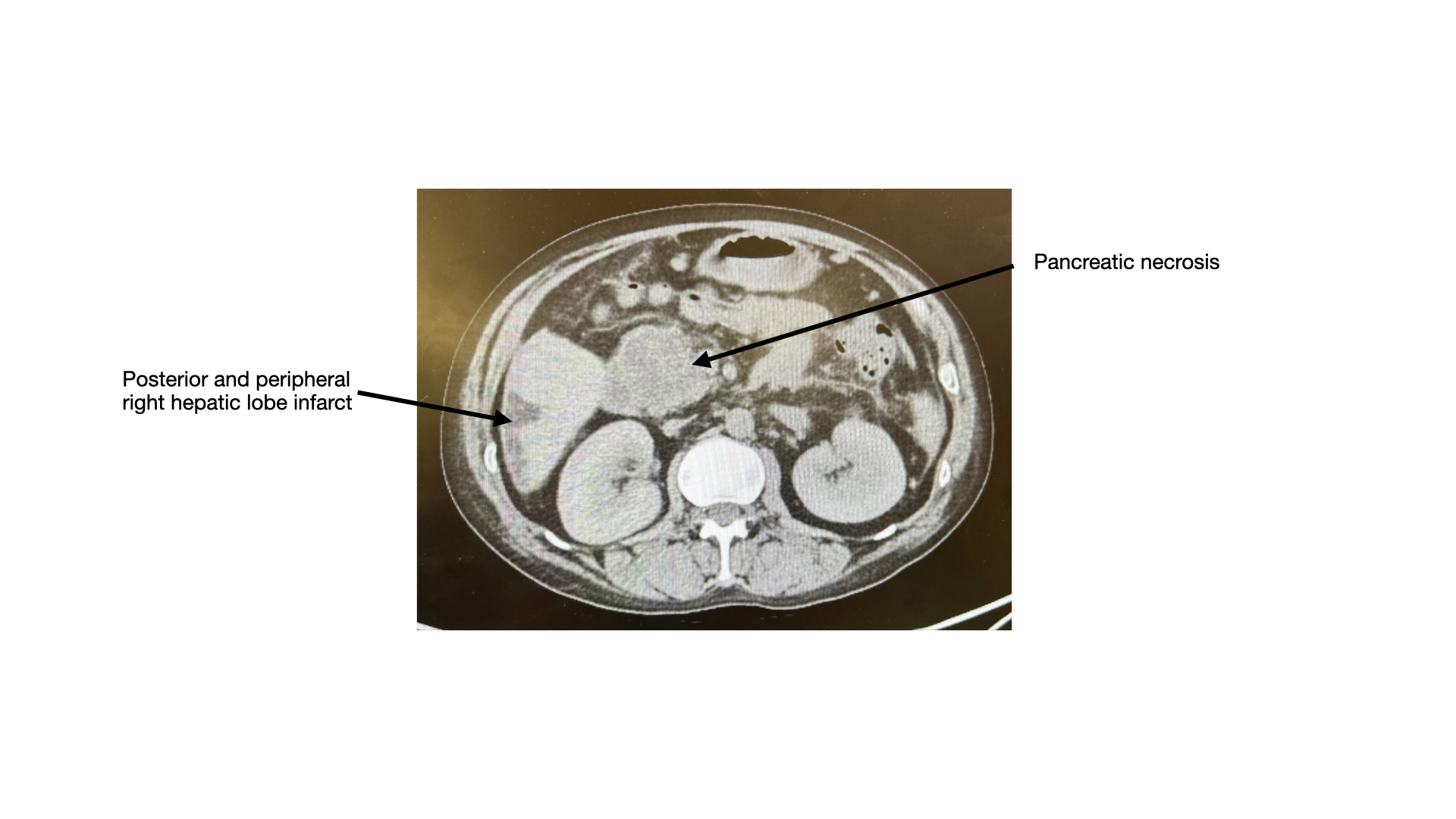
Figure: CT Abdomen and Pelvis without contrast
Disclosures:
Simran Rameshbhai Patel indicated no relevant financial relationships.
Ayesha Jamil indicated no relevant financial relationships.
Syed Mahmood indicated no relevant financial relationships.
Abhishek Agnihotri indicated no relevant financial relationships.
Simran Rameshbhai Patel, MD, Ayesha Jamil, MD, Syed Mahmood, MD, Abhishek Agnihotri, MD. P0178 - A Rapid Descent: Early Walled-Off Necrosis and Hepatic Infarction in Acute Alcoholic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

