Sunday Poster Session
Category: Biliary/Pancreas
P0173 - Diagnostic Dilemma of Groove Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Galvin Dhaliwal, MD
HCA Healthcare
Kingwood, TX
Presenting Author(s)
Galvin Dhaliwal, MD1, Wafa Mehboob, DO2, Ashvin Singh Dhaliwal, MD3, Bilal Ashraf, MD4, Aakriti Soni, MD5, Ahmed Ouni, MD6, Sushovan Guha, MD, PhD7
1HCA Healthcare, Kingwood, TX; 2HCA Healthcare Kingwood Hospital/University of Houston, Spring, TX; 3Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 4HCA Healthcare Kingwood Hospital/University of Houston, Kingwood, TX; 5HCA Houston Healthcare Kingwood, Kingwood, TX; 6HCA Healthcare, Houston, TX; 7Houston Regional Gastroenterology Institute and University of Houston, Sugar Land, TX
Introduction: Groove pancreatitis is a rare form of chronic pancreatitis that affects the pancreaticoduodenal groove, the area between the pancreatic head, duodenum, and common bile duct. It typically mimics pancreatic malignancy or duodenal disorders, making the diagnosis challenging. Although alcohol and tobacco use in middle aged men are the most common risk factors for groove pancreatitis, cases without these risk factors are increasingly recognized. We present a diagnostically complex case of groove pancreatitis in a young male with metabolic risk factors, highlighting the importance of considering this diagnosis even with atypical presentations.
Case Description/
Methods: A 31-year-old male with uncontrolled type 2 diabetes and hypertriglyceridemia (687 mg/dL) presented with one week of postprandial epigastric pain and vomiting. He reported multiple episodes of pancreatitis over the past year, managed conservatively without a definitive etiology. He denied alcohol or tobacco use, gallstones, prior surgeries, or abdominal trauma. Physical exam was pertinent for localized epigastric tenderness. Labs revealed a normal lipase level (127 U/L), liver chemistries, calcium, and IgG4 levels. A contrast-enhanced CT scan showed inflammation and early necrosis in the inferior pancreatic head with a 4.6 × 0.9 cm peripancreatic fluid collection. MRI with pancreatic protocol demonstrated duodenal wall thickening, uncinate process edema, with findings being consistent with groove pancreatitis (Figure 1, 2). There was concern for a possible obstructing lesion in the minor papilla region. He was managed conservatively with IV fluids, fenofibrate, and analgesia, with gradual clinical improvement.
Discussion: This case illustrates the diagnostic difficulty of groove pancreatitis, particularly in patients without traditional risk factors. Its imaging and clinical overlap with pancreatic malignancy often leads to delays in diagnosis or unnecessary surgical intervention. In this patient, groove pancreatitis was only identified after MRI during a recurrent flare. This case also highlights the growing understanding that metabolic factors, such as poorly controlled diabetes and hypertriglyceridemia, are important contributing factors to groove pancreatitis. Recognizing this broader risk profile may aid earlier diagnosis, reduce unnecessary procedures, and improve outcomes in similar patients.
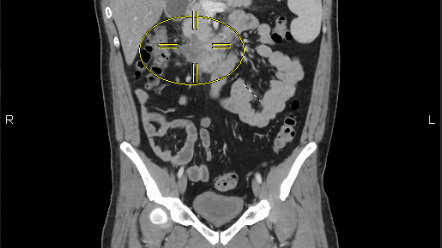
Figure: Figure 1: MRI showing abnormal thickening of the third portion of the duodenum with mild edema along the uncinate process of the pancreas
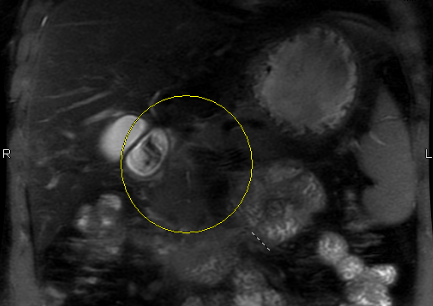
Figure: Figure 2: MRI showing abnormal thickening of the third portion of the duodenum with mild edema along the uncinate process of the pancreas
Disclosures:
Galvin Dhaliwal indicated no relevant financial relationships.
Wafa Mehboob indicated no relevant financial relationships.
Ashvin Singh Dhaliwal indicated no relevant financial relationships.
Bilal Ashraf indicated no relevant financial relationships.
Aakriti Soni indicated no relevant financial relationships.
Ahmed Ouni indicated no relevant financial relationships.
Sushovan Guha indicated no relevant financial relationships.
Galvin Dhaliwal, MD1, Wafa Mehboob, DO2, Ashvin Singh Dhaliwal, MD3, Bilal Ashraf, MD4, Aakriti Soni, MD5, Ahmed Ouni, MD6, Sushovan Guha, MD, PhD7. P0173 - Diagnostic Dilemma of Groove Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare, Kingwood, TX; 2HCA Healthcare Kingwood Hospital/University of Houston, Spring, TX; 3Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 4HCA Healthcare Kingwood Hospital/University of Houston, Kingwood, TX; 5HCA Houston Healthcare Kingwood, Kingwood, TX; 6HCA Healthcare, Houston, TX; 7Houston Regional Gastroenterology Institute and University of Houston, Sugar Land, TX
Introduction: Groove pancreatitis is a rare form of chronic pancreatitis that affects the pancreaticoduodenal groove, the area between the pancreatic head, duodenum, and common bile duct. It typically mimics pancreatic malignancy or duodenal disorders, making the diagnosis challenging. Although alcohol and tobacco use in middle aged men are the most common risk factors for groove pancreatitis, cases without these risk factors are increasingly recognized. We present a diagnostically complex case of groove pancreatitis in a young male with metabolic risk factors, highlighting the importance of considering this diagnosis even with atypical presentations.
Case Description/
Methods: A 31-year-old male with uncontrolled type 2 diabetes and hypertriglyceridemia (687 mg/dL) presented with one week of postprandial epigastric pain and vomiting. He reported multiple episodes of pancreatitis over the past year, managed conservatively without a definitive etiology. He denied alcohol or tobacco use, gallstones, prior surgeries, or abdominal trauma. Physical exam was pertinent for localized epigastric tenderness. Labs revealed a normal lipase level (127 U/L), liver chemistries, calcium, and IgG4 levels. A contrast-enhanced CT scan showed inflammation and early necrosis in the inferior pancreatic head with a 4.6 × 0.9 cm peripancreatic fluid collection. MRI with pancreatic protocol demonstrated duodenal wall thickening, uncinate process edema, with findings being consistent with groove pancreatitis (Figure 1, 2). There was concern for a possible obstructing lesion in the minor papilla region. He was managed conservatively with IV fluids, fenofibrate, and analgesia, with gradual clinical improvement.
Discussion: This case illustrates the diagnostic difficulty of groove pancreatitis, particularly in patients without traditional risk factors. Its imaging and clinical overlap with pancreatic malignancy often leads to delays in diagnosis or unnecessary surgical intervention. In this patient, groove pancreatitis was only identified after MRI during a recurrent flare. This case also highlights the growing understanding that metabolic factors, such as poorly controlled diabetes and hypertriglyceridemia, are important contributing factors to groove pancreatitis. Recognizing this broader risk profile may aid earlier diagnosis, reduce unnecessary procedures, and improve outcomes in similar patients.
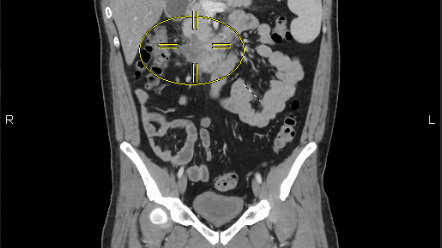
Figure: Figure 1: MRI showing abnormal thickening of the third portion of the duodenum with mild edema along the uncinate process of the pancreas
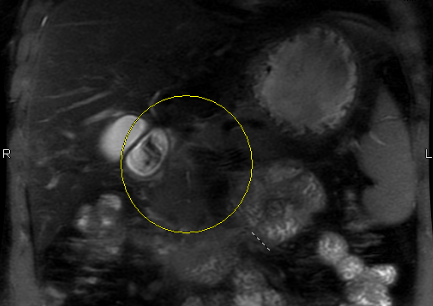
Figure: Figure 2: MRI showing abnormal thickening of the third portion of the duodenum with mild edema along the uncinate process of the pancreas
Disclosures:
Galvin Dhaliwal indicated no relevant financial relationships.
Wafa Mehboob indicated no relevant financial relationships.
Ashvin Singh Dhaliwal indicated no relevant financial relationships.
Bilal Ashraf indicated no relevant financial relationships.
Aakriti Soni indicated no relevant financial relationships.
Ahmed Ouni indicated no relevant financial relationships.
Sushovan Guha indicated no relevant financial relationships.
Galvin Dhaliwal, MD1, Wafa Mehboob, DO2, Ashvin Singh Dhaliwal, MD3, Bilal Ashraf, MD4, Aakriti Soni, MD5, Ahmed Ouni, MD6, Sushovan Guha, MD, PhD7. P0173 - Diagnostic Dilemma of Groove Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
