Sunday Poster Session
Category: Biliary/Pancreas
P0167 - Pancreatic Duct Disruption Secondary to Perforated Gastric Ulcer: A Rare Complication of Peptic Ulcer Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Aziz Eshov, DO (he/him/his)
Skagit Regional Hospital
Arlington, AR
Presenting Author(s)
Aziz Eshov, DO1, Jayanta Datta, 2, Samit Datta, MD3
1Skagit Regional Hospital, Arlington, WA; 2The Ohio State University, Columbus, OH; 3Skagit Regional Hospital., Mount Vernon, WA
Introduction: Peptic ulcer disease (PUD) is a gastrointestinal disorder characterized by mucosal damage occurring in the stomach or duodenum. Notable risk factors for PUD include smoking, alcohol consumption, and infection with H. pylori. Perforated peptic ulcer (PPU) is a serious complication of PUD observed in 2-14% of all PUD cases. In this report, we present a rare case of gastric ulcer perforation leading to a pancreatic duct leak.
Case Description/
Methods: We present the case of a 77-year-old female with a history of gastric ulcer who was admitted to the hospital due to sudden onset of epigastric abdominal pain. Initial CT abdomen revealed pneumoperitoneum, raising concerns for a perforated ulcer. Although general surgery was initially consulted, the patient was deemed a poor surgical candidate due to her comorbidities. Consequently, she was managed conservatively with proton pump inhibitors and empiric antibiotics.
A few days later, patient’s leukocytosis worsened and repeat CT abdomen demonstrated increased pneumoperitoneum with large fluid collection in the anterior upper abdomen (Figure 1). CT-guided abscess drainage revealed straw colored fluid with lipase of 14,000. Patient was not able to undergo MRCP due to previous aneurysm clips and therefore received ERCP, which identified contrast extravasation at the genu of the pancreatic duct (PD) (Figure 2). A PD stent was placed to help resolve PD leak and patient’s symptoms improved.
Discussion: PPU is a severe complication with a mortality rate ranging from 20 % - 70 %. The standard treatment for most perforations is surgical intervention. Non-operative management is typically reserved for small, uncomplicated perforations or for patients who are not suitable candidates for surgery. Well-documented complications of untreated PPU include hypovolemic shock, peritonitis, sepsis, and gastrocolic fistula. An exceptionally rare complication, PD disruption, has been reported in only one other case involving a patient who was a surgical candidate. This case report highlights the rare occurrence of pancreatic duct leak due to PPU and discusses its appropriate management in a patient who was a non-candidate. Furthermore, it illustrates the utility of abdominal fluid analysis for lipase as a diagnostic aid in detecting a PD leak in a patient who was unable to undergo MRCP.
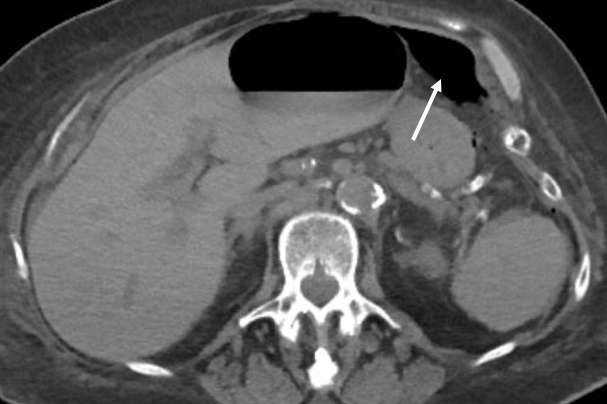
Figure: Axial CT abdomen showing pneumoperitoneum.
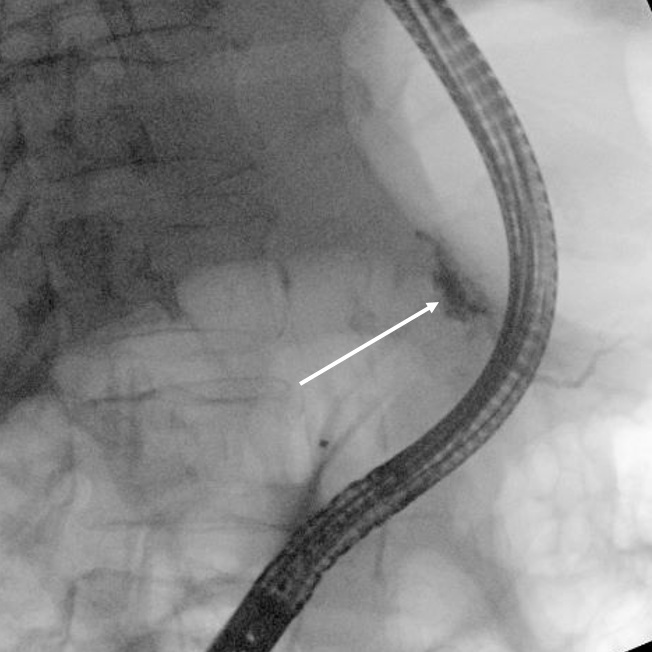
Figure: ERCP showing extravasation of contrast near the genu of the pancreatic duct.
Disclosures:
Aziz Eshov indicated no relevant financial relationships.
Jayanta Datta indicated no relevant financial relationships.
Samit Datta indicated no relevant financial relationships.
Aziz Eshov, DO1, Jayanta Datta, 2, Samit Datta, MD3. P0167 - Pancreatic Duct Disruption Secondary to Perforated Gastric Ulcer: A Rare Complication of Peptic Ulcer Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Skagit Regional Hospital, Arlington, WA; 2The Ohio State University, Columbus, OH; 3Skagit Regional Hospital., Mount Vernon, WA
Introduction: Peptic ulcer disease (PUD) is a gastrointestinal disorder characterized by mucosal damage occurring in the stomach or duodenum. Notable risk factors for PUD include smoking, alcohol consumption, and infection with H. pylori. Perforated peptic ulcer (PPU) is a serious complication of PUD observed in 2-14% of all PUD cases. In this report, we present a rare case of gastric ulcer perforation leading to a pancreatic duct leak.
Case Description/
Methods: We present the case of a 77-year-old female with a history of gastric ulcer who was admitted to the hospital due to sudden onset of epigastric abdominal pain. Initial CT abdomen revealed pneumoperitoneum, raising concerns for a perforated ulcer. Although general surgery was initially consulted, the patient was deemed a poor surgical candidate due to her comorbidities. Consequently, she was managed conservatively with proton pump inhibitors and empiric antibiotics.
A few days later, patient’s leukocytosis worsened and repeat CT abdomen demonstrated increased pneumoperitoneum with large fluid collection in the anterior upper abdomen (Figure 1). CT-guided abscess drainage revealed straw colored fluid with lipase of 14,000. Patient was not able to undergo MRCP due to previous aneurysm clips and therefore received ERCP, which identified contrast extravasation at the genu of the pancreatic duct (PD) (Figure 2). A PD stent was placed to help resolve PD leak and patient’s symptoms improved.
Discussion: PPU is a severe complication with a mortality rate ranging from 20 % - 70 %. The standard treatment for most perforations is surgical intervention. Non-operative management is typically reserved for small, uncomplicated perforations or for patients who are not suitable candidates for surgery. Well-documented complications of untreated PPU include hypovolemic shock, peritonitis, sepsis, and gastrocolic fistula. An exceptionally rare complication, PD disruption, has been reported in only one other case involving a patient who was a surgical candidate. This case report highlights the rare occurrence of pancreatic duct leak due to PPU and discusses its appropriate management in a patient who was a non-candidate. Furthermore, it illustrates the utility of abdominal fluid analysis for lipase as a diagnostic aid in detecting a PD leak in a patient who was unable to undergo MRCP.
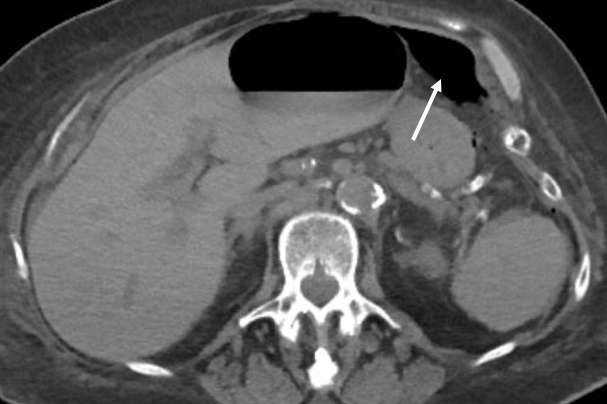
Figure: Axial CT abdomen showing pneumoperitoneum.
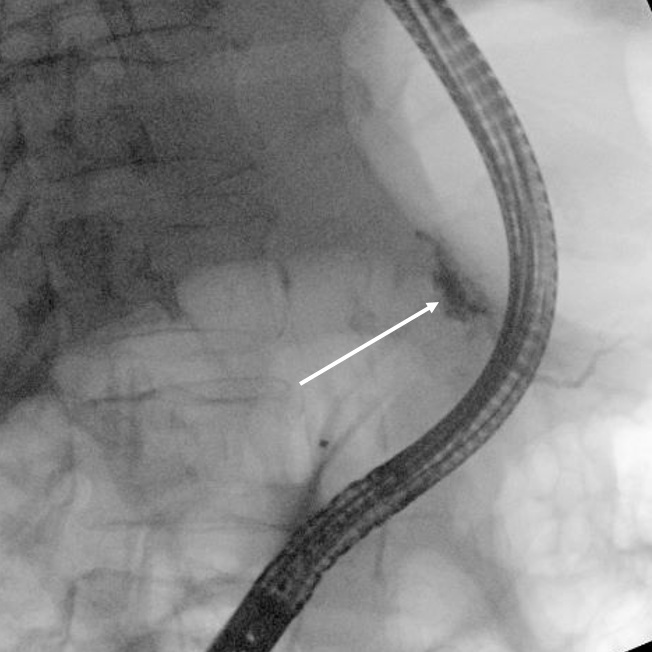
Figure: ERCP showing extravasation of contrast near the genu of the pancreatic duct.
Disclosures:
Aziz Eshov indicated no relevant financial relationships.
Jayanta Datta indicated no relevant financial relationships.
Samit Datta indicated no relevant financial relationships.
Aziz Eshov, DO1, Jayanta Datta, 2, Samit Datta, MD3. P0167 - Pancreatic Duct Disruption Secondary to Perforated Gastric Ulcer: A Rare Complication of Peptic Ulcer Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
