Sunday Poster Session
Category: Biliary/Pancreas
P0161 - Post-Pancreatitis Gastric Outlet Obstruction: A Narrow Escape
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amanda Frondella, MD (she/her/hers)
University of Connecticut Health
Scranton, PA
Presenting Author(s)
Amanda Frondella, MD1, Minh Thu T.. Nguyen, MD2, Neil Parikh, MD3
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Connecticut GI, Farmington, CT
Introduction: Gastric outlet obstruction (GOO) is a rare complication in acute pancreatitis, occurring in about 5.7% of cases. Risk factors include severe or necrotizing pancreatitis, duct disruption, and peripancreatic collections. We present a case of GOO following a first episode of acute pancreatitis, emphasizing the condition’s morbidity and the importance of close follow-up when unusual findings are present.
Case Description/
Methods: A 40-year-old male presented with nausea, vomiting, and abdominal pain. His abdomen was distended and diffusely tender. Notably, he had been hospitalized for acute pancreatitis three weeks prior, during which MRCP showed CBD dilation up to 1.3 cm without stones and mass effect from an edematous pancreatic head. A follow-up EUS was scheduled but not yet completed. CT abdomen revealed a large, ill-defined mass involving the second part of the duodenum and pancreatic head, causing GOO. A nasogastric (NG) tube was placed for gastric decompression.
The patient underwent EGD with duodenal dilation, which showed pancreatic enlargement but no discrete mass. His NG tube was removed, and he was started on a clear liquid diet, which he initially tolerated. However, due to pain, he underwent repeat CT which showed persistent GOO. Abdominal MRI showed abrupt termination of the distal CBD by a 4.8 x 4.0 cm irregular, enhancing mass, likely arising from the pancreatic head or ampulla. An EUS-guided biopsy was performed, and the patient ultimately underwent a surgical gastrojejunostomy, resulting in relief of his obstruction.
Discussion: Post-pancreatitis GOO can pose significant complications. Although imaging raised concern for malignancy, biopsy revealed only fibrous tissue and minimal duodenal mucosa, likely contaminant. Initial management of GOO includes nasogastric decompression, intravenous fluid hydration, and gradual reintroduction of diet, with the hope that obstruction resolves as inflammation subsides. In this case, due to persistent symptoms, longer-term options included endoscopic versus surgical gastrojejunostomy. Given the patient’s young age, surgical bypass was favored for its durability and the potential for a larger, more lasting anastomosis. Follow-up imaging was recommended in two months for reassessment.
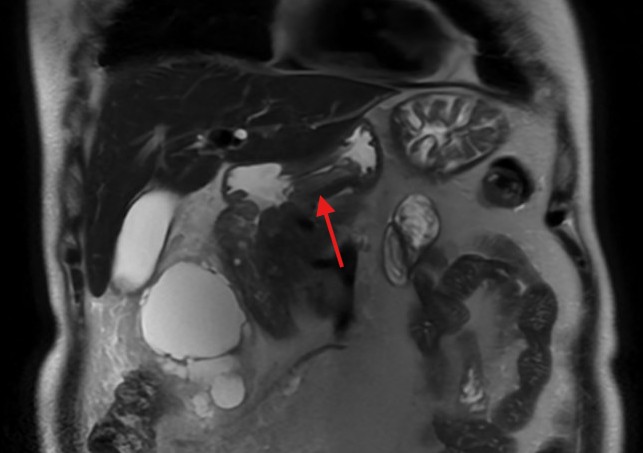
Figure: Figure 1: CT abdomen pelvis with PO and IV contrast demonstrating diffuse wall thickening of the antrum and pylorus of the stomach without any orally administered contrast extending into the duodenum.
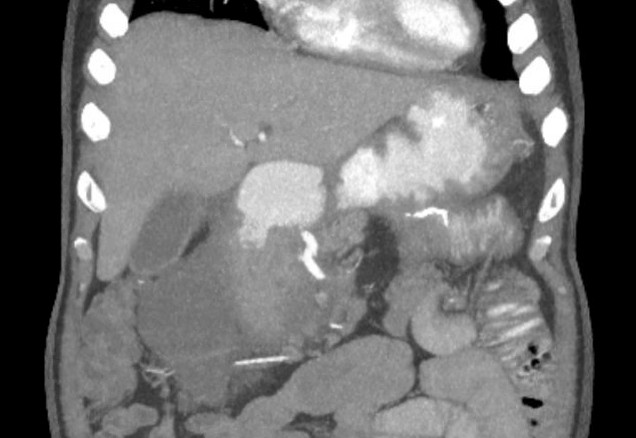
Figure: Figure 2: MRI abdomen with contrast demonstrating coronal view of duodenal stenosis by mass effect.
Disclosures:
Amanda Frondella indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Neil Parikh indicated no relevant financial relationships.
Amanda Frondella, MD1, Minh Thu T.. Nguyen, MD2, Neil Parikh, MD3. P0161 - Post-Pancreatitis Gastric Outlet Obstruction: A Narrow Escape, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Connecticut GI, Farmington, CT
Introduction: Gastric outlet obstruction (GOO) is a rare complication in acute pancreatitis, occurring in about 5.7% of cases. Risk factors include severe or necrotizing pancreatitis, duct disruption, and peripancreatic collections. We present a case of GOO following a first episode of acute pancreatitis, emphasizing the condition’s morbidity and the importance of close follow-up when unusual findings are present.
Case Description/
Methods: A 40-year-old male presented with nausea, vomiting, and abdominal pain. His abdomen was distended and diffusely tender. Notably, he had been hospitalized for acute pancreatitis three weeks prior, during which MRCP showed CBD dilation up to 1.3 cm without stones and mass effect from an edematous pancreatic head. A follow-up EUS was scheduled but not yet completed. CT abdomen revealed a large, ill-defined mass involving the second part of the duodenum and pancreatic head, causing GOO. A nasogastric (NG) tube was placed for gastric decompression.
The patient underwent EGD with duodenal dilation, which showed pancreatic enlargement but no discrete mass. His NG tube was removed, and he was started on a clear liquid diet, which he initially tolerated. However, due to pain, he underwent repeat CT which showed persistent GOO. Abdominal MRI showed abrupt termination of the distal CBD by a 4.8 x 4.0 cm irregular, enhancing mass, likely arising from the pancreatic head or ampulla. An EUS-guided biopsy was performed, and the patient ultimately underwent a surgical gastrojejunostomy, resulting in relief of his obstruction.
Discussion: Post-pancreatitis GOO can pose significant complications. Although imaging raised concern for malignancy, biopsy revealed only fibrous tissue and minimal duodenal mucosa, likely contaminant. Initial management of GOO includes nasogastric decompression, intravenous fluid hydration, and gradual reintroduction of diet, with the hope that obstruction resolves as inflammation subsides. In this case, due to persistent symptoms, longer-term options included endoscopic versus surgical gastrojejunostomy. Given the patient’s young age, surgical bypass was favored for its durability and the potential for a larger, more lasting anastomosis. Follow-up imaging was recommended in two months for reassessment.
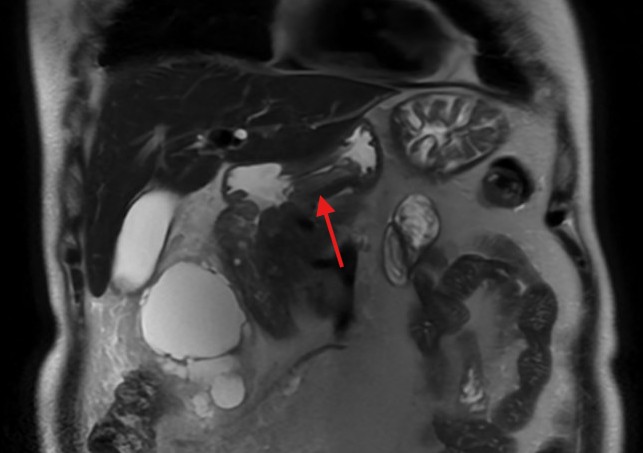
Figure: Figure 1: CT abdomen pelvis with PO and IV contrast demonstrating diffuse wall thickening of the antrum and pylorus of the stomach without any orally administered contrast extending into the duodenum.
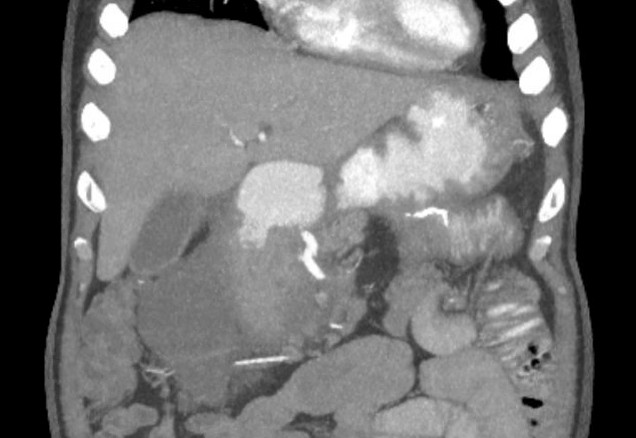
Figure: Figure 2: MRI abdomen with contrast demonstrating coronal view of duodenal stenosis by mass effect.
Disclosures:
Amanda Frondella indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Neil Parikh indicated no relevant financial relationships.
Amanda Frondella, MD1, Minh Thu T.. Nguyen, MD2, Neil Parikh, MD3. P0161 - Post-Pancreatitis Gastric Outlet Obstruction: A Narrow Escape, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
