Sunday Poster Session
Category: Biliary/Pancreas
P0155 - Malignancy Masquerade: An Atypical Care of Autoimmune Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Jeffrey R. Liu, DO (he/him/his)
University of California San Francisco - Fresno
Fresno, CA
Presenting Author(s)
Jeffrey R. Liu, DO1, Sindhu Chadalawada, MD2, Marina Roytman, MD3
1University of California San Francisco - Fresno, Fresno, CA; 2UCSF Fresno, Fresno, CA; 3Hepatology Fellowship, UCSF Fresno, Fresno, CA
Introduction: Type 1 autoimmune pancreatitis (T1-AIP) is a distinct subtype of chronic pancreatitis mediated by immunoglobin-4 (IgG4) characterized by histologic findings of storiform fibrosis and obliterative phlebitis. It presents as painless obstructive jaundice, generalized abdominal pain and weight loss, often mimicking the presentation of pancreatic adenocarcinoma. We present an atypical case of type 1 autoimmune pancreatitis.
Case Description/
Methods: A 67-year-old male with a history of type 2 diabetes mellitus presented with 4-months of progressive, pressure like epigastric pain, and unintentional weight loss of 35 lbs. Initial laboratory studies were significant for elevated liver enzymes: AST 714 U/L, ALT 981 U/L, alkaline phosphatase 613 U/L, and total bilirubin of 2.5 mg/dL. Tumor makers including alpha-fetoprotein, carcinoembryonic antigen, and CA 19-9 were negative. Serum IgG4 was elevated at 300.7 mg/dL. Single phase contrast CT abdomen and pelvis showed an ill-defined 3.7 cm pancreatic head mass with intrahepatic, common bile duct, and pancreatic duct dilatation along with mild retroperitoneal adenopathy. Given concern for malignancy, he underwent endoscopic ultrasound which showed a 4.2 x 3.3 cm irregular mass abutting and compressing the main portal vein suggesting invasion. Fine needle aspiration revealed nonspecific focal fibrosis, scant inflammatory cells, crushed plasma cells, lymphocytes and endothelial cells. IgG4 staining highlighted a few plasma cells, however, this was limited by crush artifact. Steroids were initiated twice daily for four weeks. Multiphasic contrast CT abdomen and pelvis 2 months later showed reduction of the mass to 3.1 x 3.1 cm with improvement in pancreatic duct dilation along with reduction in serum IgG4 level to 94.8 mg/dL. He continued to improve on oral prednisone therapy with resolution of the pancreatic mass and normalization of liver tests within five months.
Discussion: Autoimmune pancreatitis and pancreatic adenocarcinoma often present similarly with painless jaundice, abdominal pain, and weight loss. Given the temporal relationship between the steroid therapy and rapid clinical and radiographic resolution of the mass, our patient’s diagnosis was consistent with AIP despite inconclusive biopsy findings. While biopsy samples aid with diagnosis, there often can be false-negative results depending on the operator and sampling. Continued monitoring of serum IgG4 and close follow-up remain a cornerstone in the long-term management of patients with T1-AIP.
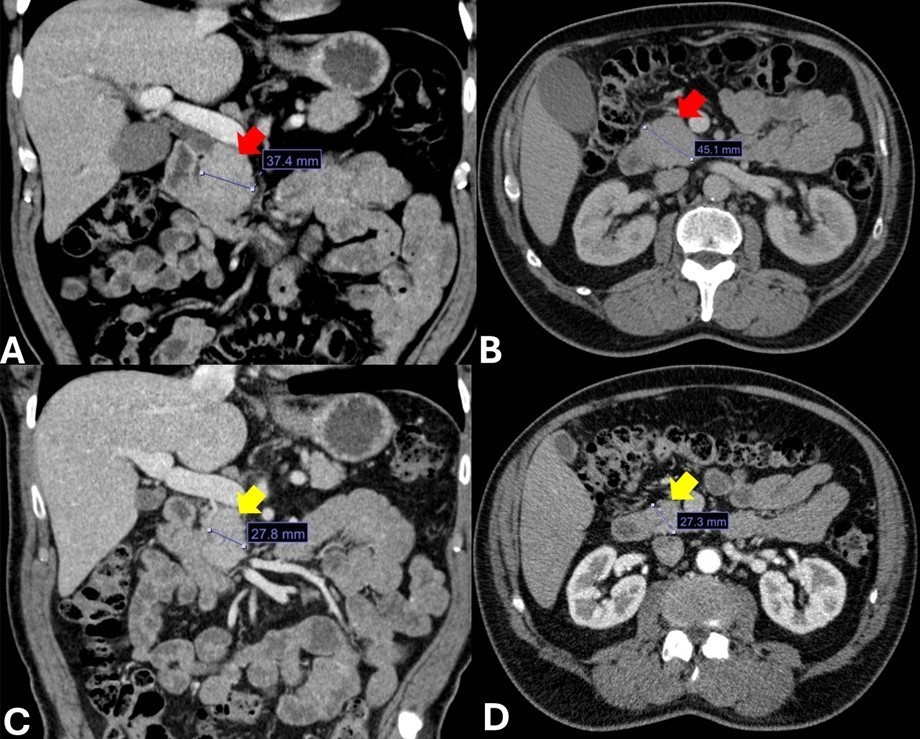
Figure: Figure 1. CT Abdomen and Pelvis of Pancreatic Mass
A-B) Coronal & Transverse Sections of Pancreatic Head Mass: 4.5x3.7 cm
C-D) Post-Steroid Therapy, Coronal & Transverse Sections of Mass: 2.7x2.7 cm
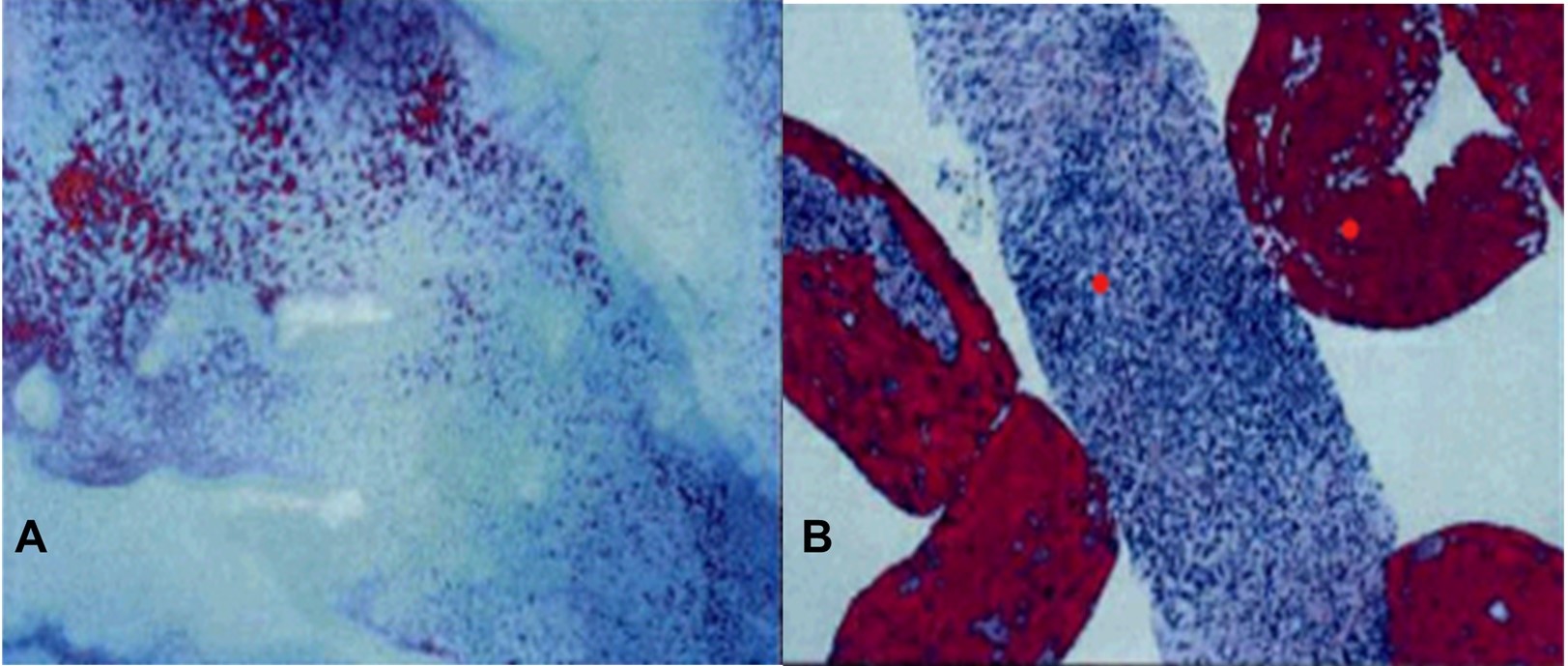
Figure: Figure 2. Fine Needle Aspiration Biopsy Samples
A-B) Crushed plasma cells, lymphocytes and endothelial cells with scattered biliary duct and scattered pancreatic acini, consistent with chronic pancreatitis
Disclosures:
Jeffrey Liu indicated no relevant financial relationships.
Sindhu Chadalawada indicated no relevant financial relationships.
Marina Roytman: Gilead – Speakers Bureau. Ipsen – Advisory Committee/Board Member. Madrigal – Speakers Bureau. Salix – Speakers Bureau.
Jeffrey R. Liu, DO1, Sindhu Chadalawada, MD2, Marina Roytman, MD3. P0155 - Malignancy Masquerade: An Atypical Care of Autoimmune Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California San Francisco - Fresno, Fresno, CA; 2UCSF Fresno, Fresno, CA; 3Hepatology Fellowship, UCSF Fresno, Fresno, CA
Introduction: Type 1 autoimmune pancreatitis (T1-AIP) is a distinct subtype of chronic pancreatitis mediated by immunoglobin-4 (IgG4) characterized by histologic findings of storiform fibrosis and obliterative phlebitis. It presents as painless obstructive jaundice, generalized abdominal pain and weight loss, often mimicking the presentation of pancreatic adenocarcinoma. We present an atypical case of type 1 autoimmune pancreatitis.
Case Description/
Methods: A 67-year-old male with a history of type 2 diabetes mellitus presented with 4-months of progressive, pressure like epigastric pain, and unintentional weight loss of 35 lbs. Initial laboratory studies were significant for elevated liver enzymes: AST 714 U/L, ALT 981 U/L, alkaline phosphatase 613 U/L, and total bilirubin of 2.5 mg/dL. Tumor makers including alpha-fetoprotein, carcinoembryonic antigen, and CA 19-9 were negative. Serum IgG4 was elevated at 300.7 mg/dL. Single phase contrast CT abdomen and pelvis showed an ill-defined 3.7 cm pancreatic head mass with intrahepatic, common bile duct, and pancreatic duct dilatation along with mild retroperitoneal adenopathy. Given concern for malignancy, he underwent endoscopic ultrasound which showed a 4.2 x 3.3 cm irregular mass abutting and compressing the main portal vein suggesting invasion. Fine needle aspiration revealed nonspecific focal fibrosis, scant inflammatory cells, crushed plasma cells, lymphocytes and endothelial cells. IgG4 staining highlighted a few plasma cells, however, this was limited by crush artifact. Steroids were initiated twice daily for four weeks. Multiphasic contrast CT abdomen and pelvis 2 months later showed reduction of the mass to 3.1 x 3.1 cm with improvement in pancreatic duct dilation along with reduction in serum IgG4 level to 94.8 mg/dL. He continued to improve on oral prednisone therapy with resolution of the pancreatic mass and normalization of liver tests within five months.
Discussion: Autoimmune pancreatitis and pancreatic adenocarcinoma often present similarly with painless jaundice, abdominal pain, and weight loss. Given the temporal relationship between the steroid therapy and rapid clinical and radiographic resolution of the mass, our patient’s diagnosis was consistent with AIP despite inconclusive biopsy findings. While biopsy samples aid with diagnosis, there often can be false-negative results depending on the operator and sampling. Continued monitoring of serum IgG4 and close follow-up remain a cornerstone in the long-term management of patients with T1-AIP.
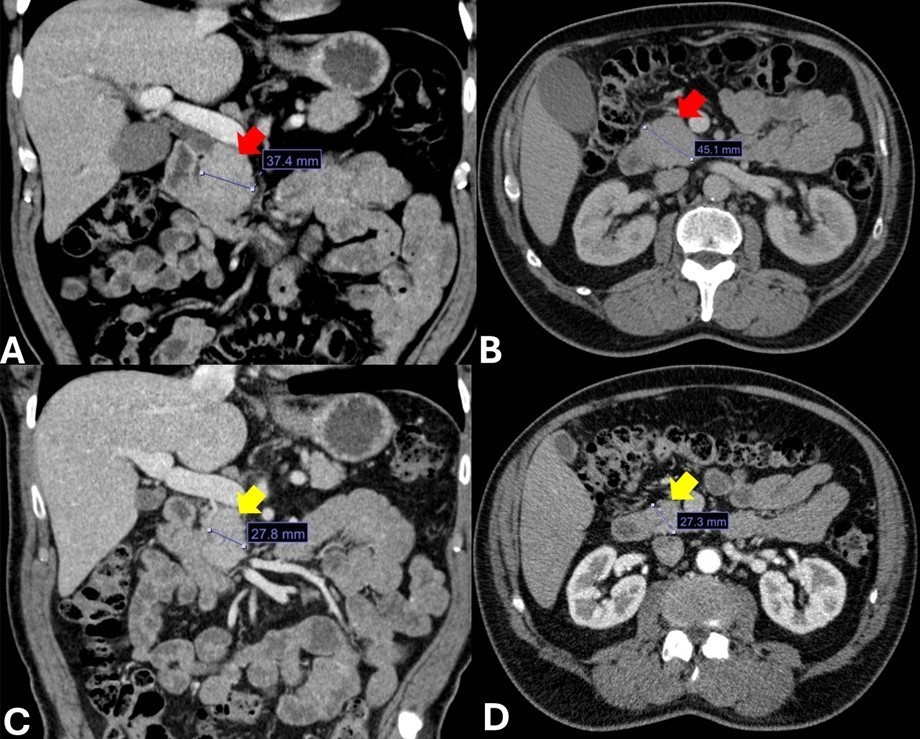
Figure: Figure 1. CT Abdomen and Pelvis of Pancreatic Mass
A-B) Coronal & Transverse Sections of Pancreatic Head Mass: 4.5x3.7 cm
C-D) Post-Steroid Therapy, Coronal & Transverse Sections of Mass: 2.7x2.7 cm
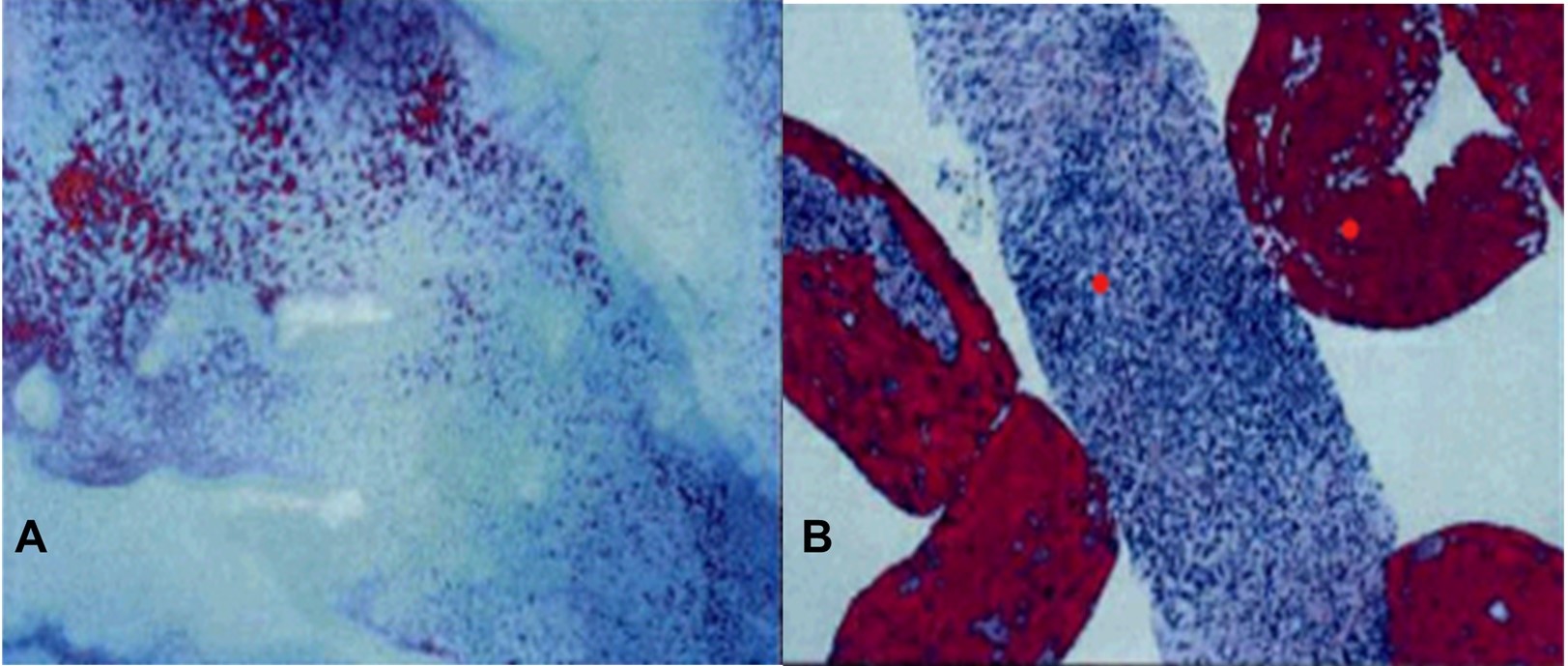
Figure: Figure 2. Fine Needle Aspiration Biopsy Samples
A-B) Crushed plasma cells, lymphocytes and endothelial cells with scattered biliary duct and scattered pancreatic acini, consistent with chronic pancreatitis
Disclosures:
Jeffrey Liu indicated no relevant financial relationships.
Sindhu Chadalawada indicated no relevant financial relationships.
Marina Roytman: Gilead – Speakers Bureau. Ipsen – Advisory Committee/Board Member. Madrigal – Speakers Bureau. Salix – Speakers Bureau.
Jeffrey R. Liu, DO1, Sindhu Chadalawada, MD2, Marina Roytman, MD3. P0155 - Malignancy Masquerade: An Atypical Care of Autoimmune Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

