Sunday Poster Session
Category: Biliary/Pancreas
P0145 - A Rare Complication of Gallstone Pancreatitis: Cholecystocolonic Fistula
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Gregory Capelli, DO
Aurora Healthcare
Milwaukee, WI
Presenting Author(s)
Gregory Capelli, DO, Adil Ghafoor, MD, Nalini Guda, MD, FACG
Aurora Healthcare, Milwaukee, WI
Introduction: Cholecystocolonic fistulas are rare, occurring in less than 0.5% of patients undergoing cholecystectomy. However, when they do develop, they can lead to complications such as colonic perforation, gallstone ileus, and infection. Here, we present a case of a patient who developed a cholecystocolonic fistula alongside gallstone-induced pancreatitis.
Case Description/
Methods: An 81-year-old woman with a history of hyperlipidemia, and hypertension presented to the emergency department with acute onset abdominal pain. Laboratory results revealed a total bilirubin of 1.0 mg/dL, AST of 103 U/L, ALT of 119 U/L, ALP of 880 U/L, lipase of 6,421 U/L, and a WBC count of 11.8 K/mcL. Physical examination showed tenderness in the epigastric area, without guarding or rigidity. Gallbladder ultrasound revealed a 7mm common bile duct diameter and questionable pneumobilia. CT of the abdomen demonstrated an air-fluid level in the pancreatic head/uncinate process, along with small-volume pneumobilia. MRCP confirmed the presence of pneumobilia and suspected a communication between the gallbladder and the hepatic flexure of the colon, raising concern for a cholecystocolonic fistula. Several filling defects were also identified within the extrahepatic bile ducts, including a 1 cm dependent filling defect in the distal common bile duct. Given these findings, the patient underwent colonoscopy and ERCP. During ERCP, contrast was observed flowing from the gallbladder into the colon under fluoroscopy. Balloon sweep of the common bile duct revealed multiple small stones and one larger stone measuring approximately 12mm. Colonoscopy identified a fistulous connection between the gallbladder and right colon, which was marked with a tattoo. The following day, the patient underwent a successful right hemicolectomy, cholecystectomy, and takedown of the cholecystocolonic fistula using the previously placed tattoo as a guide. Postoperatively, liver chemistries improved in a stepwise fashion. The patient tolerated the procedure well, with no complications, and was discharged in stable condition.
Discussion: Cholecystocolonic fistulas are rare complications of gallstone disease, typically presenting with large gallstones that compress the gallbladder and colon. This case highlights the clinical presentation, diagnostic evaluation, and surgical management of this unusual complication. Timely identification and appropriate management are crucial in preventing further complications such as gallstone ileus or bowel perforation.
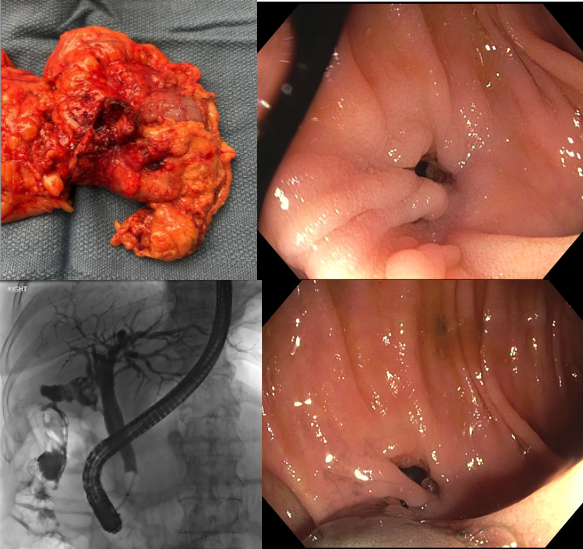
Figure: Upper left: Resected right colon and gallbladder specimen demonstrating the cholecystocolonic fistulous tract. Upper right: Colonoscopic image showing the internal opening of the cholecystocolonic fistula. Lower right: Colonoscopic image highlighting the fistulous opening with adjacent tattoo placement for intraoperative localization. Lower left: Fluoroscopic image from ERCP showing contrast extravasation from the gallbladder into the colon, confirming the fistulous communication.
Disclosures:
Gregory Capelli indicated no relevant financial relationships.
Adil Ghafoor indicated no relevant financial relationships.
Nalini Guda: boston scientific – Consultant. Braintree – Consultant. Lupin Pharmaceuticals, India – Consultant. Medtronic India – Consultant. Pentax – Consultant.
Gregory Capelli, DO, Adil Ghafoor, MD, Nalini Guda, MD, FACG. P0145 - A Rare Complication of Gallstone Pancreatitis: Cholecystocolonic Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Aurora Healthcare, Milwaukee, WI
Introduction: Cholecystocolonic fistulas are rare, occurring in less than 0.5% of patients undergoing cholecystectomy. However, when they do develop, they can lead to complications such as colonic perforation, gallstone ileus, and infection. Here, we present a case of a patient who developed a cholecystocolonic fistula alongside gallstone-induced pancreatitis.
Case Description/
Methods: An 81-year-old woman with a history of hyperlipidemia, and hypertension presented to the emergency department with acute onset abdominal pain. Laboratory results revealed a total bilirubin of 1.0 mg/dL, AST of 103 U/L, ALT of 119 U/L, ALP of 880 U/L, lipase of 6,421 U/L, and a WBC count of 11.8 K/mcL. Physical examination showed tenderness in the epigastric area, without guarding or rigidity. Gallbladder ultrasound revealed a 7mm common bile duct diameter and questionable pneumobilia. CT of the abdomen demonstrated an air-fluid level in the pancreatic head/uncinate process, along with small-volume pneumobilia. MRCP confirmed the presence of pneumobilia and suspected a communication between the gallbladder and the hepatic flexure of the colon, raising concern for a cholecystocolonic fistula. Several filling defects were also identified within the extrahepatic bile ducts, including a 1 cm dependent filling defect in the distal common bile duct. Given these findings, the patient underwent colonoscopy and ERCP. During ERCP, contrast was observed flowing from the gallbladder into the colon under fluoroscopy. Balloon sweep of the common bile duct revealed multiple small stones and one larger stone measuring approximately 12mm. Colonoscopy identified a fistulous connection between the gallbladder and right colon, which was marked with a tattoo. The following day, the patient underwent a successful right hemicolectomy, cholecystectomy, and takedown of the cholecystocolonic fistula using the previously placed tattoo as a guide. Postoperatively, liver chemistries improved in a stepwise fashion. The patient tolerated the procedure well, with no complications, and was discharged in stable condition.
Discussion: Cholecystocolonic fistulas are rare complications of gallstone disease, typically presenting with large gallstones that compress the gallbladder and colon. This case highlights the clinical presentation, diagnostic evaluation, and surgical management of this unusual complication. Timely identification and appropriate management are crucial in preventing further complications such as gallstone ileus or bowel perforation.
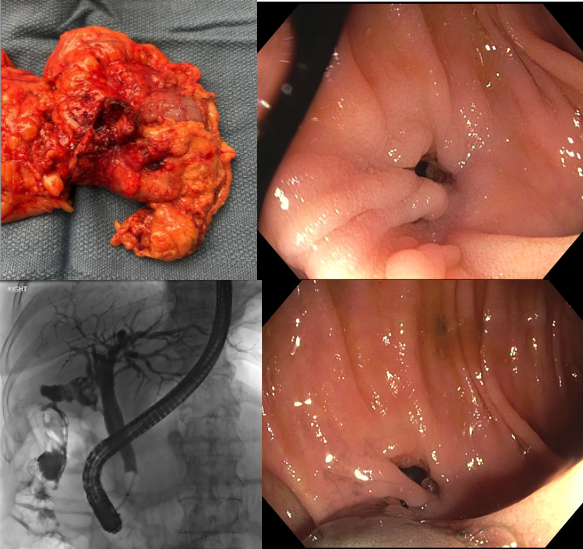
Figure: Upper left: Resected right colon and gallbladder specimen demonstrating the cholecystocolonic fistulous tract. Upper right: Colonoscopic image showing the internal opening of the cholecystocolonic fistula. Lower right: Colonoscopic image highlighting the fistulous opening with adjacent tattoo placement for intraoperative localization. Lower left: Fluoroscopic image from ERCP showing contrast extravasation from the gallbladder into the colon, confirming the fistulous communication.
Disclosures:
Gregory Capelli indicated no relevant financial relationships.
Adil Ghafoor indicated no relevant financial relationships.
Nalini Guda: boston scientific – Consultant. Braintree – Consultant. Lupin Pharmaceuticals, India – Consultant. Medtronic India – Consultant. Pentax – Consultant.
Gregory Capelli, DO, Adil Ghafoor, MD, Nalini Guda, MD, FACG. P0145 - A Rare Complication of Gallstone Pancreatitis: Cholecystocolonic Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
