Sunday Poster Session
Category: Biliary/Pancreas
P0143 - Ampullary Adenoma as a Rare Cause of Acute Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JA
John K. Appiah, MD
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
John K. Appiah, MD1, Cherukuri Sreehari, MD1, Nikita Garg, MD1, John Samies, DO1, Amit Sohagia, MD2
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Geisinger Community Medical Center, Scranton, PA
Introduction: While gallstones and alcohol are the most common causes of acute pancreatitis, up to 30% of cases remain idiopathic. Rarely, obstructing ampullary lesions may underlie pancreatic inflammation. We present a case of idiopathic pancreatitis ultimately attributed to an ampullary tubulovillous adenoma, highlighting the role of advanced endoscopic evaluation.
Case Description/
Methods: A 67-year-old man presented with acute epigastric pain radiating to the back and constipation. He reported no history of alcohol use, high-risk medications, recent procedures, or family history of pancreatitis. Laboratory tests showed elevated lipase (124 U/L), leukocytosis (WBC 15.23), and CRP (262 mg/L). Liver enzymes, triglycerides, calcium, IgG4, and ethanol screen were unremarkable. CT imaging demonstrated peripancreatic stranding. Abdominal ultrasound revealed no gallstones or biliary dilation. The patient improved with supportive care and was discharged with a presumptive diagnosis of idiopathic pancreatitis. Given the absence of a clear etiology, further outpatient evaluation was pursued. MRI showed a small peripancreatic fluid collection. Esophagogastroduodenoscopy (EGD) revealed a polypoid ampulla; endoscopic ultrasound (EUS) showed mild pancreatic parenchymal changes and a cystic lesion in the body with benign features. Endoscopic retrograde cholangiopancreatography (ERCP) with snare papillectomy was performed, and a pancreatic duct stent was placed. Pathology revealed a tubulovillous adenoma without high-grade dysplasia or malignancy. The patient remained asymptomatic and was scheduled for surveillance.
Discussion: Ampullary adenomas are an uncommon and often overlooked cause of acute pancreatitis, particularly in the absence of jaundice or biliary dilation. Their ability to intermittently obstruct the pancreatic duct underscores the importance of a thorough endoscopic workup in cases initially labeled as idiopathic. Cross-sectional imaging may miss subtle ampullary lesions, making direct visualization via EGD and detailed assessment with EUS critical for diagnosis. ERCP not only confirms the diagnosis but also allows for therapeutic intervention. Endoscopic papillectomy is a safe and effective alternative to surgical resection for select ampullary adenomas, with low morbidity and recurrence when coupled with appropriate surveillance. This case reinforces the value of a stepwise diagnostic approach and highlights the expanding role of endoscopic therapy in managing benign ampullary pathology.

Figure: Figure 1. Endoscopic image demonstrating a polypoid ampullary lesion consistent with a tubulovillous adenoma, identified during evaluation for idiopathic pancreatitis.
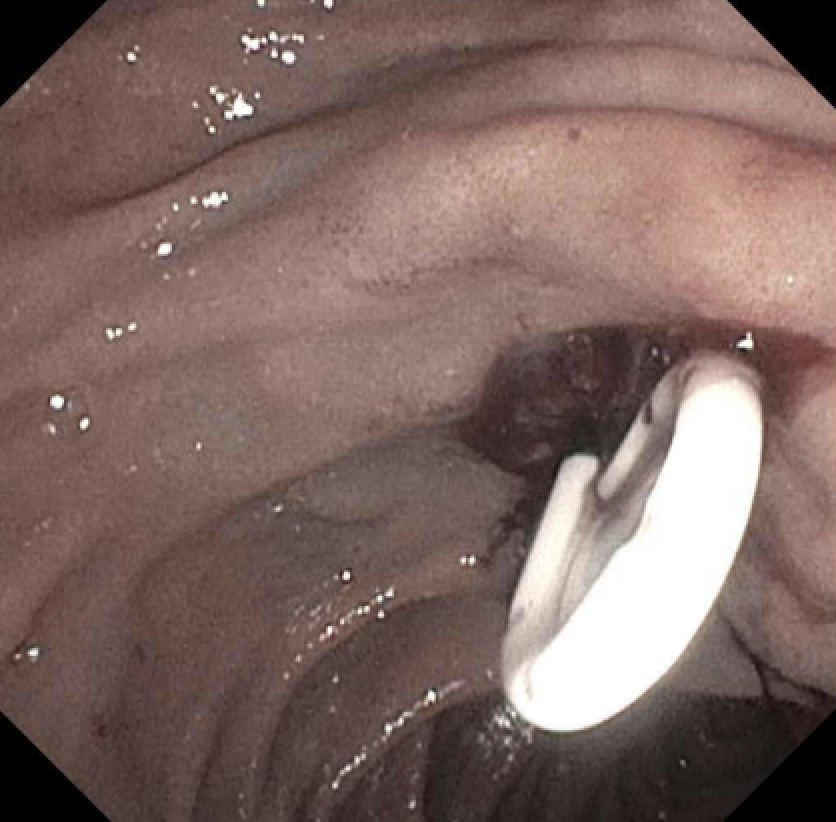
Figure: Figure 2. Endoscopic image after hot snare papillectomy of the ampullary lesion, showing the post-resection site with placement of a prophylactic pancreatic duct stent to reduce the risk of post-ERCP pancreatitis.
Disclosures:
John Appiah indicated no relevant financial relationships.
Cherukuri Sreehari indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
John Samies indicated no relevant financial relationships.
Amit Sohagia indicated no relevant financial relationships.
John K. Appiah, MD1, Cherukuri Sreehari, MD1, Nikita Garg, MD1, John Samies, DO1, Amit Sohagia, MD2. P0143 - Ampullary Adenoma as a Rare Cause of Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Geisinger Community Medical Center, Scranton, PA
Introduction: While gallstones and alcohol are the most common causes of acute pancreatitis, up to 30% of cases remain idiopathic. Rarely, obstructing ampullary lesions may underlie pancreatic inflammation. We present a case of idiopathic pancreatitis ultimately attributed to an ampullary tubulovillous adenoma, highlighting the role of advanced endoscopic evaluation.
Case Description/
Methods: A 67-year-old man presented with acute epigastric pain radiating to the back and constipation. He reported no history of alcohol use, high-risk medications, recent procedures, or family history of pancreatitis. Laboratory tests showed elevated lipase (124 U/L), leukocytosis (WBC 15.23), and CRP (262 mg/L). Liver enzymes, triglycerides, calcium, IgG4, and ethanol screen were unremarkable. CT imaging demonstrated peripancreatic stranding. Abdominal ultrasound revealed no gallstones or biliary dilation. The patient improved with supportive care and was discharged with a presumptive diagnosis of idiopathic pancreatitis. Given the absence of a clear etiology, further outpatient evaluation was pursued. MRI showed a small peripancreatic fluid collection. Esophagogastroduodenoscopy (EGD) revealed a polypoid ampulla; endoscopic ultrasound (EUS) showed mild pancreatic parenchymal changes and a cystic lesion in the body with benign features. Endoscopic retrograde cholangiopancreatography (ERCP) with snare papillectomy was performed, and a pancreatic duct stent was placed. Pathology revealed a tubulovillous adenoma without high-grade dysplasia or malignancy. The patient remained asymptomatic and was scheduled for surveillance.
Discussion: Ampullary adenomas are an uncommon and often overlooked cause of acute pancreatitis, particularly in the absence of jaundice or biliary dilation. Their ability to intermittently obstruct the pancreatic duct underscores the importance of a thorough endoscopic workup in cases initially labeled as idiopathic. Cross-sectional imaging may miss subtle ampullary lesions, making direct visualization via EGD and detailed assessment with EUS critical for diagnosis. ERCP not only confirms the diagnosis but also allows for therapeutic intervention. Endoscopic papillectomy is a safe and effective alternative to surgical resection for select ampullary adenomas, with low morbidity and recurrence when coupled with appropriate surveillance. This case reinforces the value of a stepwise diagnostic approach and highlights the expanding role of endoscopic therapy in managing benign ampullary pathology.

Figure: Figure 1. Endoscopic image demonstrating a polypoid ampullary lesion consistent with a tubulovillous adenoma, identified during evaluation for idiopathic pancreatitis.
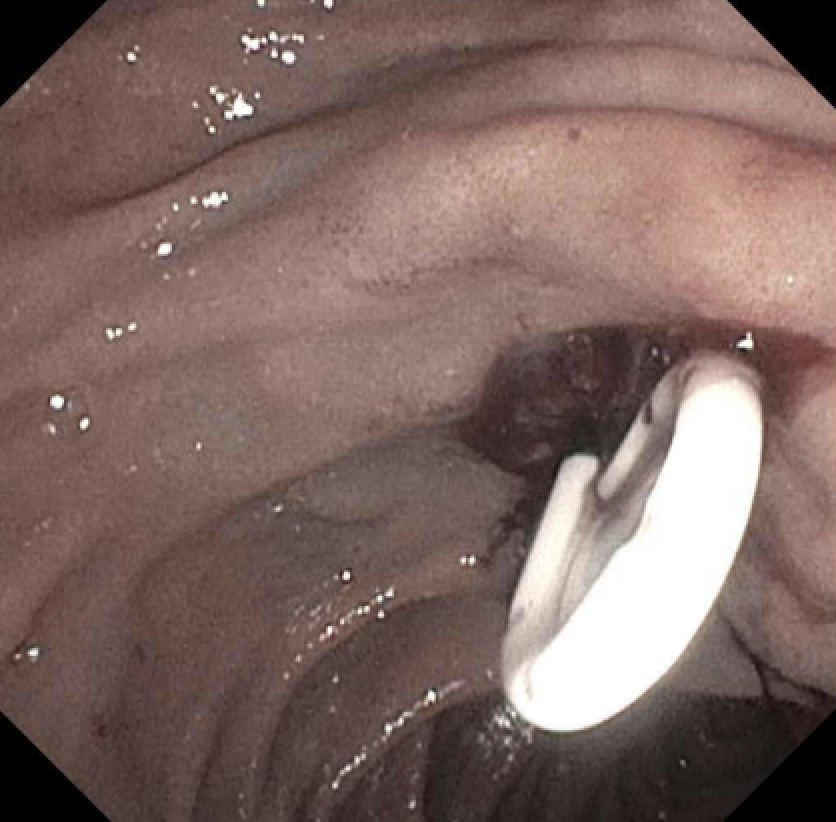
Figure: Figure 2. Endoscopic image after hot snare papillectomy of the ampullary lesion, showing the post-resection site with placement of a prophylactic pancreatic duct stent to reduce the risk of post-ERCP pancreatitis.
Disclosures:
John Appiah indicated no relevant financial relationships.
Cherukuri Sreehari indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
John Samies indicated no relevant financial relationships.
Amit Sohagia indicated no relevant financial relationships.
John K. Appiah, MD1, Cherukuri Sreehari, MD1, Nikita Garg, MD1, John Samies, DO1, Amit Sohagia, MD2. P0143 - Ampullary Adenoma as a Rare Cause of Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
