Sunday Poster Session
Category: Biliary/Pancreas
P0116 - Type 1 Autoimmune Pancreatitis Masquerading as Malignancy in a Resource-Limited Tertiary Hospital in Guatemala
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Abel Sanchez, MD, MSc (he/him/his)
Hospital Roosevelt / Gastri-k
Guatemala City, San Marcos, Guatemala
Presenting Author(s)
Bryan Torres, MD1, Jorge Obando, 2, Abel Sanchez, MD, MSc3
1Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Chimaltenango, Guatemala; 3Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Autoimmune pancreatitis (AIP) type 1 is a rare fibroinflammatory disorder that often mimics pancreatic or biliary malignancies. Its diagnosis remains particularly challenging in resource-limited settings, where access to advanced diagnostics and awareness of IgG4-related disease is limited
Case Description/
Methods: A 49-year-old Guatemalan male presented to a public tertiary-level hospital with four months of fluctuating painless jaundice, asthenia, and fatigue. He had no significant surgical history and reported past alcohol use. Initial labs revealed a cholestatic pattern. Abdominal ultrasound showed intrahepatic bile duct dilation and biliary sludge. Follow-up MRCP revealed a diffusely enlarged “sausage-shaped” pancreas with increased T2 signal and preserved peripancreatic fat. Serum IgG4 was markedly elevated at 337 mg/dL (normal: 10–140). Endoscopic ultrasound demonstrated hypoechoic enlargement of the pancreatic parenchyma and infiltration of the pancreatic head into the portal-splenic-mesenteric confluence. The main bile duct was dilated (9.3 mm) with thickened, hyperechoic walls. EUS-guided fine-needle biopsy revealed preserved lobular structure, reduced acinar cells, abundant fibrosis, lymphoplasmacytic infiltrate, and absence of malignancy. Based on clinical, radiologic, and histologic findings, a diagnosis of AIP type 1 was made. Oral prednisone (40 mg/day) was initiated and gradually tapered over six months. The patient achieved full clinical and radiologic remission
Discussion: This case illustrates the diagnostic complexity of AIP type 1 in a low-income country, where access to IgG4 testing, EUS, and histology is often limited. In our Guatemalan public hospital, multidisciplinary collaboration enabled early diagnosis, avoiding misdiagnosis and unnecessary surgery. Awareness of AIP in atypical presentations of obstructive jaundice is crucial—especially in limited-resource environments—to ensure accurate treatment and prevent overtreatment. This report emphasizes the importance of global diagnostic equity in rare GI diseases
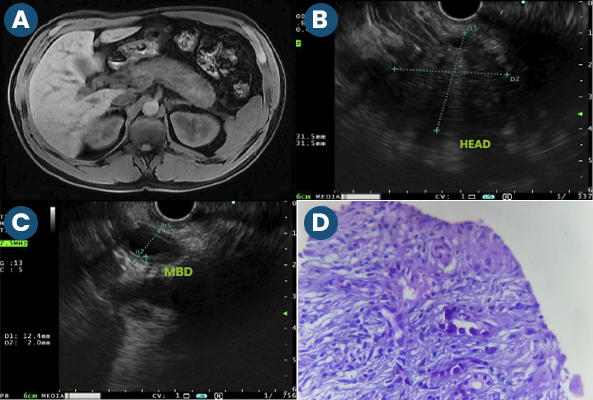
Figure: Figure 1. A: MRI showing diffusely enlarged “sausage-shaped” pancreas with T2 hyperintensity. B: Endoscopic ultrasound (EUS) view of the pancreatic head showing hypoechoic enlargement. C: EUS showing dilated main bile duct (MBD) measuring 9.3 mm with thickened walls. D: Pancreatic biopsy with abundant fibrosis and lymphoplasmacytic infiltrate (H&E stain, 40x)
Disclosures:
Bryan Torres indicated no relevant financial relationships.
Jorge Obando indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Bryan Torres, MD1, Jorge Obando, 2, Abel Sanchez, MD, MSc3. P0116 - Type 1 Autoimmune Pancreatitis Masquerading as Malignancy in a Resource-Limited Tertiary Hospital in Guatemala, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Chimaltenango, Guatemala; 3Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Autoimmune pancreatitis (AIP) type 1 is a rare fibroinflammatory disorder that often mimics pancreatic or biliary malignancies. Its diagnosis remains particularly challenging in resource-limited settings, where access to advanced diagnostics and awareness of IgG4-related disease is limited
Case Description/
Methods: A 49-year-old Guatemalan male presented to a public tertiary-level hospital with four months of fluctuating painless jaundice, asthenia, and fatigue. He had no significant surgical history and reported past alcohol use. Initial labs revealed a cholestatic pattern. Abdominal ultrasound showed intrahepatic bile duct dilation and biliary sludge. Follow-up MRCP revealed a diffusely enlarged “sausage-shaped” pancreas with increased T2 signal and preserved peripancreatic fat. Serum IgG4 was markedly elevated at 337 mg/dL (normal: 10–140). Endoscopic ultrasound demonstrated hypoechoic enlargement of the pancreatic parenchyma and infiltration of the pancreatic head into the portal-splenic-mesenteric confluence. The main bile duct was dilated (9.3 mm) with thickened, hyperechoic walls. EUS-guided fine-needle biopsy revealed preserved lobular structure, reduced acinar cells, abundant fibrosis, lymphoplasmacytic infiltrate, and absence of malignancy. Based on clinical, radiologic, and histologic findings, a diagnosis of AIP type 1 was made. Oral prednisone (40 mg/day) was initiated and gradually tapered over six months. The patient achieved full clinical and radiologic remission
Discussion: This case illustrates the diagnostic complexity of AIP type 1 in a low-income country, where access to IgG4 testing, EUS, and histology is often limited. In our Guatemalan public hospital, multidisciplinary collaboration enabled early diagnosis, avoiding misdiagnosis and unnecessary surgery. Awareness of AIP in atypical presentations of obstructive jaundice is crucial—especially in limited-resource environments—to ensure accurate treatment and prevent overtreatment. This report emphasizes the importance of global diagnostic equity in rare GI diseases
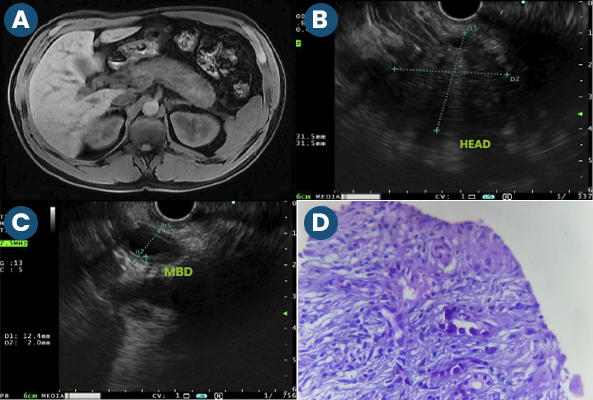
Figure: Figure 1. A: MRI showing diffusely enlarged “sausage-shaped” pancreas with T2 hyperintensity. B: Endoscopic ultrasound (EUS) view of the pancreatic head showing hypoechoic enlargement. C: EUS showing dilated main bile duct (MBD) measuring 9.3 mm with thickened walls. D: Pancreatic biopsy with abundant fibrosis and lymphoplasmacytic infiltrate (H&E stain, 40x)
Disclosures:
Bryan Torres indicated no relevant financial relationships.
Jorge Obando indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Bryan Torres, MD1, Jorge Obando, 2, Abel Sanchez, MD, MSc3. P0116 - Type 1 Autoimmune Pancreatitis Masquerading as Malignancy in a Resource-Limited Tertiary Hospital in Guatemala, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
