Sunday Poster Session
Category: Biliary/Pancreas
P0114 - Semaglutide-Induced FATAL Acute Necrotizing Pancreatitis Complicated by ARDS and Septic Shock
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Deepak Kumar, MBBS, MD (he/him/his)
Northwell Health
Port Jefferson, NY
Presenting Author(s)
Deepak Kumar, MBBS, MD1, Fareeha Ajmal, MD2, Lindsey Donnelly, MD3, Sunny Kumar, MD4, Janta Devi Ukrani, MBBS, MD1, Ramona Rajapakse, MD, FACG3
1Northwell Health, Port Jefferson, NY; 2Northwell at MATHER Hospital, Port Jefferson, NY; 3Mather Hospital, Northwell Health, Port Jefferson, NY; 4Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Acute pancreatitis is a serious condition with various etiologies, including rare drug-induced cases. Semaglutide, a glucagon-like peptide-1 receptor agonist used for diabetes and weight management, is infrequently associated with pancreatitis. We report a fatal case of semaglutide-induced acute necrotizing pancreatitis complicated by acute respiratory distress syndrome (ARDS) and septic shock, highlighting its clinical course and management challenges.
Case Description/
Methods: A 67-year-old female presented with severe epigastric pain radiating to the left flank and back, accompanied by bilious vomiting for 4 hours. She had a history of hypertension, osteoporosis, dyslipidemia, anxiety, and a pancreatic uncinate cystic lesion (10 x 8 mm, likely intraductal papillary mucinous neoplasm) with main pancreatic duct dilatation (4–5 mm) noted on MRI/MRCP 10 months prior. She had minimal alcohol use and a remote smoking history. Medications included lisinopril, risedronate, rosuvastatin, alprazolam, and semaglutide, started 1–2 weeks earlier, with the last dose 2 days before presentation. Initial findings included leukocytosis, elevated lactate, lipase >3000 U/L, and normal liver/renal function. Imaging confirmed acute necrotizing pancreatitis with proximal pancreatic hypoenhancement and ileus but no peripancreatic fluid collections. She received aggressive IV hydration and broad-spectrum antibiotics for suspected semaglutide-induced pancreatitis. Despite pain management, she developed oliguria, severe metabolic acidosis, respiratory alkalosis, elevated creatinine, and hypocalcemia. Progressive dyspnea led to ICU transfer for ARDS and septic shock. Repeat imaging showed worsening pancreatitis with new ascites. Hemodialysis was initiated for acute renal failure, and ventricular tachycardia was managed with amiodarone and cardioversion. Despite interventions, including sodium bicarbonate and adjusted sedation, her condition deteriorated. After family discussions, a DNR/DNI order was established, and she succumbed to septic shock and ARDS, likely triggered by semaglutide-induced pancreatitis.
Discussion: This case highlights the rare but severe risk of semaglutide-associated necrotizing pancreatitis, particularly in patients with pre-existing pancreatic pathology. Clinicians should exercise caution when prescribing GLP-1 receptor agonists to such patients and monitor closely for early pancreatitis symptoms to prevent catastrophic outcomes.
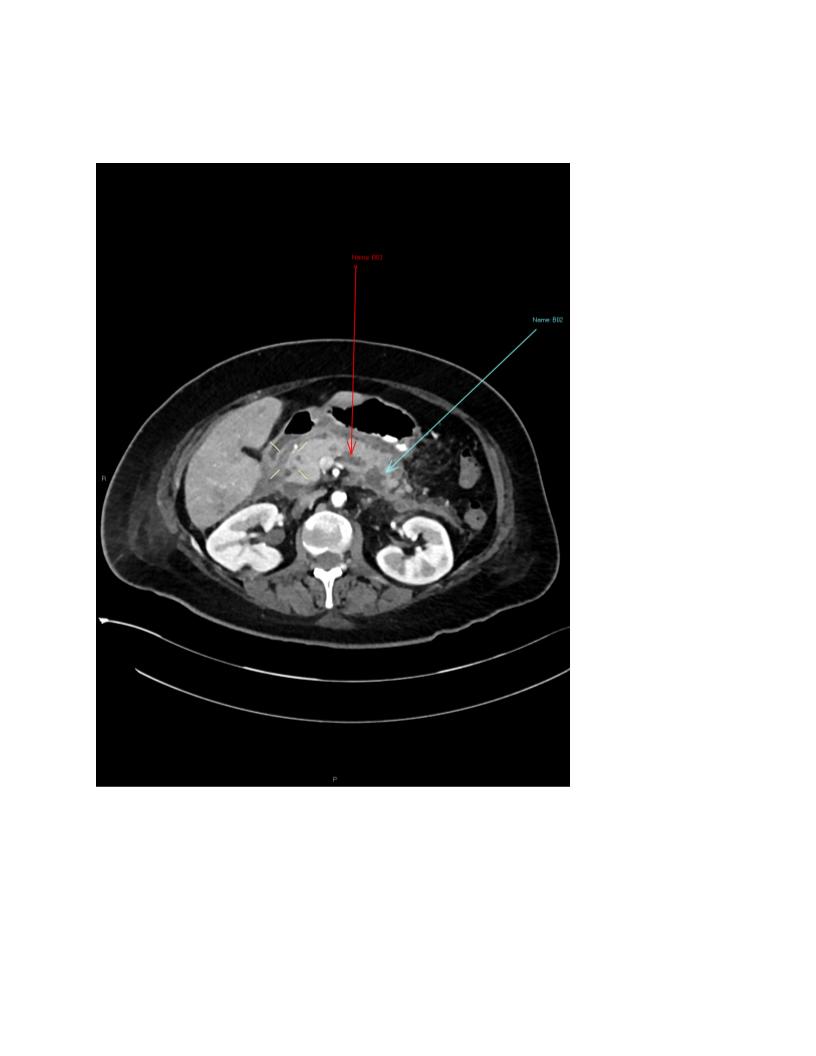
Figure: Acute pancreatitis with proximal pancreatic hypoenhancement, indicating necrosis, without peripancreatic fluid collections.
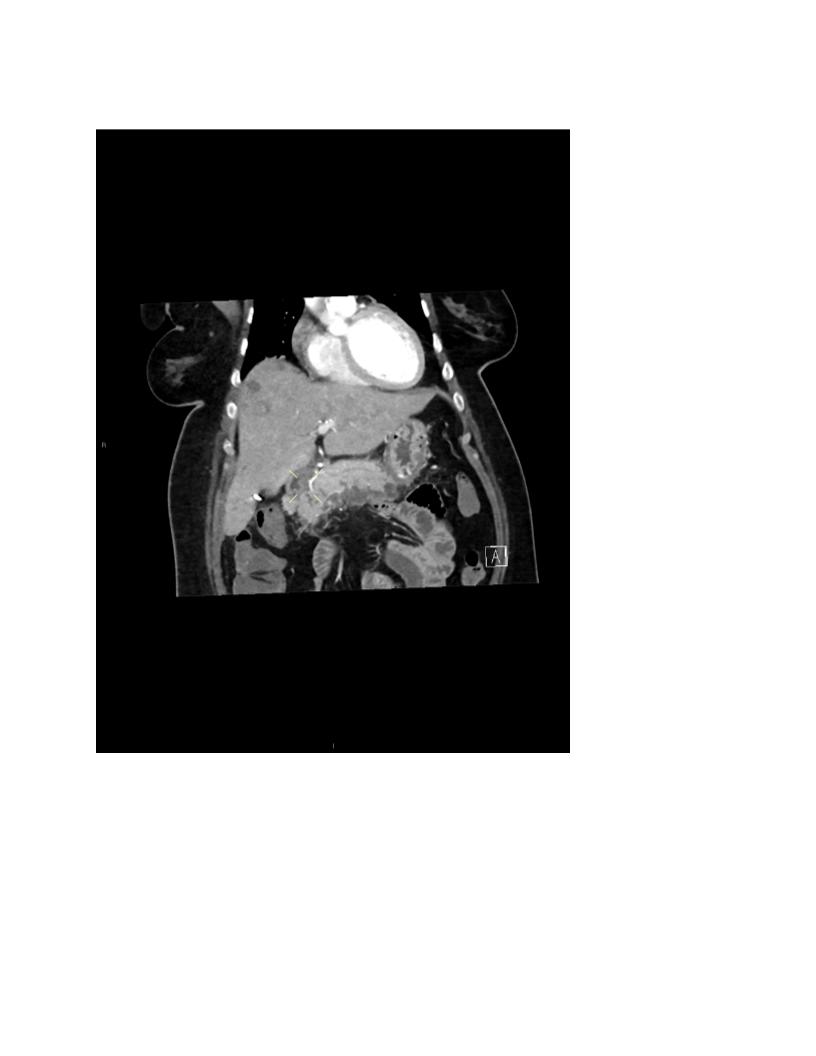
Figure: Coronal view showing Acute pancreatitis with proximal pancreatic hypoenhancement, indicating necrosis, without peripancreatic fluid collections.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Fareeha Ajmal indicated no relevant financial relationships.
Lindsey Donnelly indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Fareeha Ajmal, MD2, Lindsey Donnelly, MD3, Sunny Kumar, MD4, Janta Devi Ukrani, MBBS, MD1, Ramona Rajapakse, MD, FACG3. P0114 - Semaglutide-Induced FATAL Acute Necrotizing Pancreatitis Complicated by ARDS and Septic Shock, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Port Jefferson, NY; 2Northwell at MATHER Hospital, Port Jefferson, NY; 3Mather Hospital, Northwell Health, Port Jefferson, NY; 4Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Acute pancreatitis is a serious condition with various etiologies, including rare drug-induced cases. Semaglutide, a glucagon-like peptide-1 receptor agonist used for diabetes and weight management, is infrequently associated with pancreatitis. We report a fatal case of semaglutide-induced acute necrotizing pancreatitis complicated by acute respiratory distress syndrome (ARDS) and septic shock, highlighting its clinical course and management challenges.
Case Description/
Methods: A 67-year-old female presented with severe epigastric pain radiating to the left flank and back, accompanied by bilious vomiting for 4 hours. She had a history of hypertension, osteoporosis, dyslipidemia, anxiety, and a pancreatic uncinate cystic lesion (10 x 8 mm, likely intraductal papillary mucinous neoplasm) with main pancreatic duct dilatation (4–5 mm) noted on MRI/MRCP 10 months prior. She had minimal alcohol use and a remote smoking history. Medications included lisinopril, risedronate, rosuvastatin, alprazolam, and semaglutide, started 1–2 weeks earlier, with the last dose 2 days before presentation. Initial findings included leukocytosis, elevated lactate, lipase >3000 U/L, and normal liver/renal function. Imaging confirmed acute necrotizing pancreatitis with proximal pancreatic hypoenhancement and ileus but no peripancreatic fluid collections. She received aggressive IV hydration and broad-spectrum antibiotics for suspected semaglutide-induced pancreatitis. Despite pain management, she developed oliguria, severe metabolic acidosis, respiratory alkalosis, elevated creatinine, and hypocalcemia. Progressive dyspnea led to ICU transfer for ARDS and septic shock. Repeat imaging showed worsening pancreatitis with new ascites. Hemodialysis was initiated for acute renal failure, and ventricular tachycardia was managed with amiodarone and cardioversion. Despite interventions, including sodium bicarbonate and adjusted sedation, her condition deteriorated. After family discussions, a DNR/DNI order was established, and she succumbed to septic shock and ARDS, likely triggered by semaglutide-induced pancreatitis.
Discussion: This case highlights the rare but severe risk of semaglutide-associated necrotizing pancreatitis, particularly in patients with pre-existing pancreatic pathology. Clinicians should exercise caution when prescribing GLP-1 receptor agonists to such patients and monitor closely for early pancreatitis symptoms to prevent catastrophic outcomes.
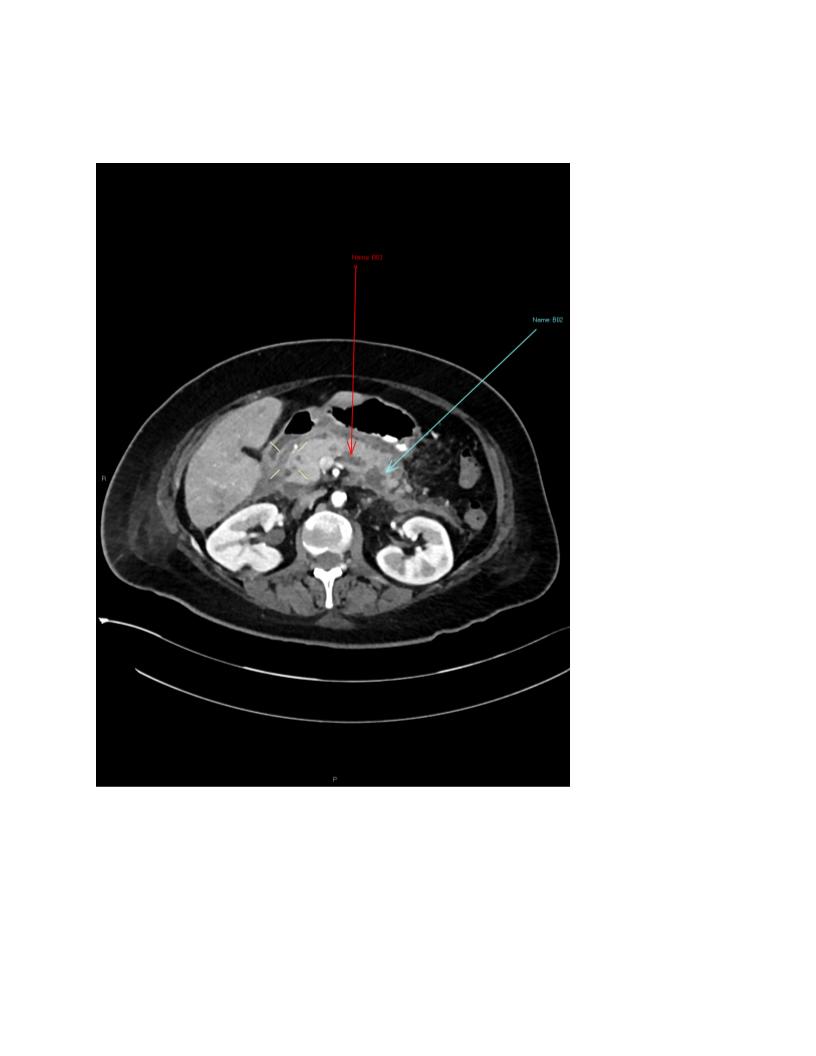
Figure: Acute pancreatitis with proximal pancreatic hypoenhancement, indicating necrosis, without peripancreatic fluid collections.
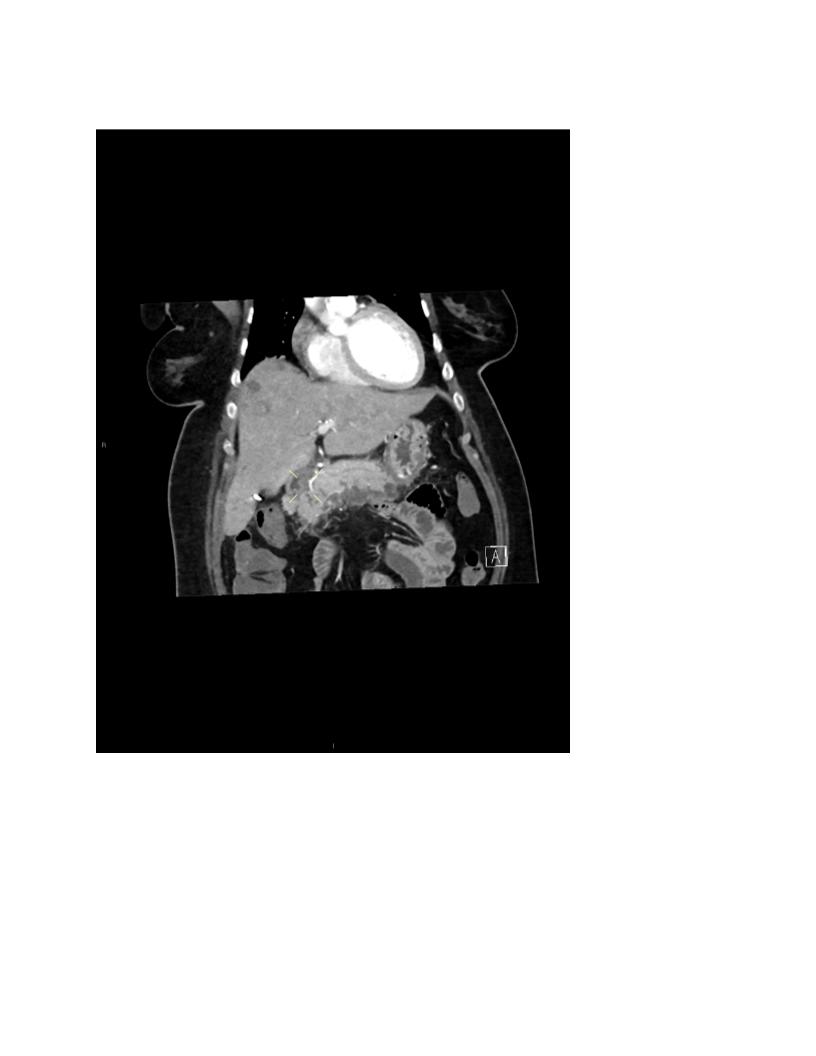
Figure: Coronal view showing Acute pancreatitis with proximal pancreatic hypoenhancement, indicating necrosis, without peripancreatic fluid collections.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Fareeha Ajmal indicated no relevant financial relationships.
Lindsey Donnelly indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Fareeha Ajmal, MD2, Lindsey Donnelly, MD3, Sunny Kumar, MD4, Janta Devi Ukrani, MBBS, MD1, Ramona Rajapakse, MD, FACG3. P0114 - Semaglutide-Induced FATAL Acute Necrotizing Pancreatitis Complicated by ARDS and Septic Shock, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
