Sunday Poster Session
Category: Biliary/Pancreas
P0113 - Ozempic-Induced Pancreatitis Leading to Recurrent Flares, Evolving Pseudocysts, and Superinfection: A Multidisciplinary Management Challenge
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Deepak Kumar, MBBS, MD (he/him/his)
Northwell Health
Port Jefferson, NY
Presenting Author(s)
Deepak Kumar, MBBS, MD1, Sunny Kumar, MD2, Anila Mahesh, MD3, Janta Devi Ukrani, MBBS, MD1, Kishore Kumar, MD4, Jyoti Yadav, MD5, Jaspreet Singh, MD6
1Northwell Health, Port Jefferson, NY; 2Wright Center for Graduate Medical Education, Scranton, PA; 3Geisinger Wyoming Valley Medical Center, Duryea, PA; 4Geisinger Community Medical Center, Scranton, PA; 5The Wright Center for Graduate Medical Education, Scranton, PA; 6Northwell Health, Bay Shore, NY
Introduction: Pancreatic pseudocysts commonly develop after acute pancreatitis but may become symptomatic or infected, warranting intervention. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), including semaglutide (Ozempic), have been associated with rare cases of drug-induced pancreatitis. We present a complex case of recurrent pancreatitis in a patient with pancreatic cystic lesions, including suspected pseudocysts, evolving into superinfection requiring necrosectomy and drainage.
Case Description/
Methods: A 55-year-old woman with a history of type 2 diabetes, hypothyroidism, GERD, and Guillain-Barré syndrome presented with severe epigastric pain. Labs revealed lipase 2623 U/L. CT abdomen showed peripancreatic fat stranding and a 3.8 cm hypodense lesion in the pancreatic body. Prior MRCP had shown multiple stable 2–3 cm pancreatic cysts. She had a known history of Ozempic-induced pancreatitis with suspected pseudocyst and mildly elevated CA 19-9. Previous EUS revealed a 2.7 cm cyst in the pancreatic body without ductal communication; FNA was deferred.
Following initial improvement, she was readmitted with worsening abdominal pain. Repeat imaging showed interval necrosis in the pancreatic neck and tail with evolving low-density peripancreatic collections. MRI confirmed enlargement of a pancreatic tail pseudocyst to 4.2 cm with surrounding fat necrosis.
She was later readmitted for pneumonia and sepsis. CT abdomen revealed further pseudocyst enlargement and mild diverticulitis. Blood cultures grew Streptococcus constellatus, raising concern for infected pseudocyst. She had no peritoneal signs. Multidisciplinary consultation involving Infectious Disease, Gastroenterology, Surgery, and Interventional Radiology was obtained. She underwent EGD/EUS-guided drainage with cyst debridement and stent placement. Necrosectomy was not required. She improved with antibiotics and pancreatic enzyme replacement therapy.
Discussion: This case illustrates the potential for GLP-1 agonist–associated pancreatitis to evolve into chronic, recurrent pancreatitis with pseudocyst formation and superinfection. Diagnostic imaging including MRI and EUS is critical for characterizing cystic lesions and guiding management. Superinfection, suggested by positive cultures and clinical deterioration, mandates timely multidisciplinary intervention. Endoscopic drainage followed by surgical washout was successful in this case. Long-term surveillance remains essential, given the underlying cystic lesions and prior incomplete follow-up.
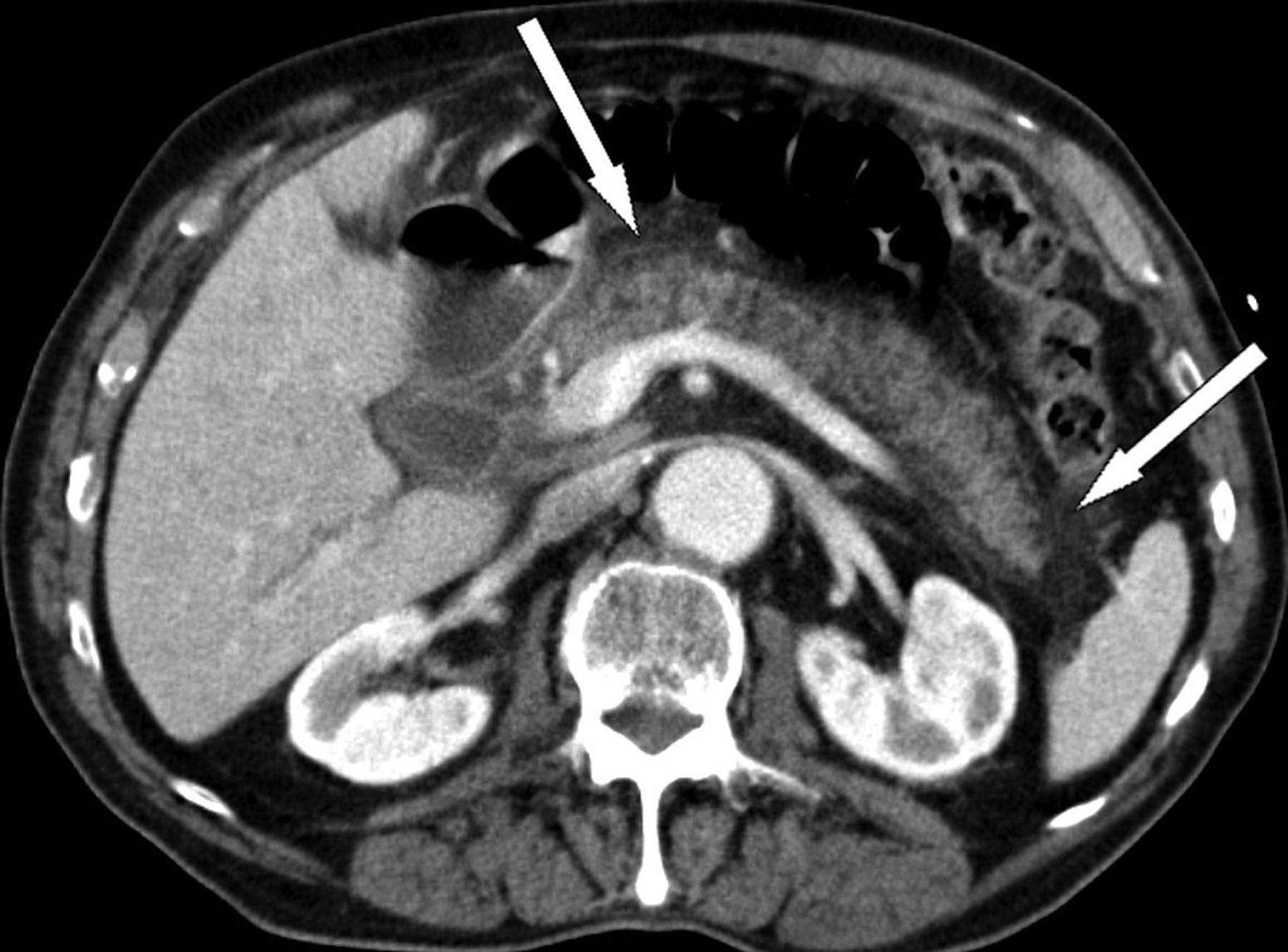
Figure: CT abdomen showed peripancreatic fat stranding and a 3.8 cm hypodense lesion in the pancreatic body.

Figure: CT abdomen revealed further Pancreatic Pseudocyst enlargement and mild diverticulitis.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Anila Mahesh indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Kishore Kumar indicated no relevant financial relationships.
Jyoti Yadav indicated no relevant financial relationships.
Jaspreet Singh indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Sunny Kumar, MD2, Anila Mahesh, MD3, Janta Devi Ukrani, MBBS, MD1, Kishore Kumar, MD4, Jyoti Yadav, MD5, Jaspreet Singh, MD6. P0113 - Ozempic-Induced Pancreatitis Leading to Recurrent Flares, Evolving Pseudocysts, and Superinfection: A Multidisciplinary Management Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Port Jefferson, NY; 2Wright Center for Graduate Medical Education, Scranton, PA; 3Geisinger Wyoming Valley Medical Center, Duryea, PA; 4Geisinger Community Medical Center, Scranton, PA; 5The Wright Center for Graduate Medical Education, Scranton, PA; 6Northwell Health, Bay Shore, NY
Introduction: Pancreatic pseudocysts commonly develop after acute pancreatitis but may become symptomatic or infected, warranting intervention. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), including semaglutide (Ozempic), have been associated with rare cases of drug-induced pancreatitis. We present a complex case of recurrent pancreatitis in a patient with pancreatic cystic lesions, including suspected pseudocysts, evolving into superinfection requiring necrosectomy and drainage.
Case Description/
Methods: A 55-year-old woman with a history of type 2 diabetes, hypothyroidism, GERD, and Guillain-Barré syndrome presented with severe epigastric pain. Labs revealed lipase 2623 U/L. CT abdomen showed peripancreatic fat stranding and a 3.8 cm hypodense lesion in the pancreatic body. Prior MRCP had shown multiple stable 2–3 cm pancreatic cysts. She had a known history of Ozempic-induced pancreatitis with suspected pseudocyst and mildly elevated CA 19-9. Previous EUS revealed a 2.7 cm cyst in the pancreatic body without ductal communication; FNA was deferred.
Following initial improvement, she was readmitted with worsening abdominal pain. Repeat imaging showed interval necrosis in the pancreatic neck and tail with evolving low-density peripancreatic collections. MRI confirmed enlargement of a pancreatic tail pseudocyst to 4.2 cm with surrounding fat necrosis.
She was later readmitted for pneumonia and sepsis. CT abdomen revealed further pseudocyst enlargement and mild diverticulitis. Blood cultures grew Streptococcus constellatus, raising concern for infected pseudocyst. She had no peritoneal signs. Multidisciplinary consultation involving Infectious Disease, Gastroenterology, Surgery, and Interventional Radiology was obtained. She underwent EGD/EUS-guided drainage with cyst debridement and stent placement. Necrosectomy was not required. She improved with antibiotics and pancreatic enzyme replacement therapy.
Discussion: This case illustrates the potential for GLP-1 agonist–associated pancreatitis to evolve into chronic, recurrent pancreatitis with pseudocyst formation and superinfection. Diagnostic imaging including MRI and EUS is critical for characterizing cystic lesions and guiding management. Superinfection, suggested by positive cultures and clinical deterioration, mandates timely multidisciplinary intervention. Endoscopic drainage followed by surgical washout was successful in this case. Long-term surveillance remains essential, given the underlying cystic lesions and prior incomplete follow-up.
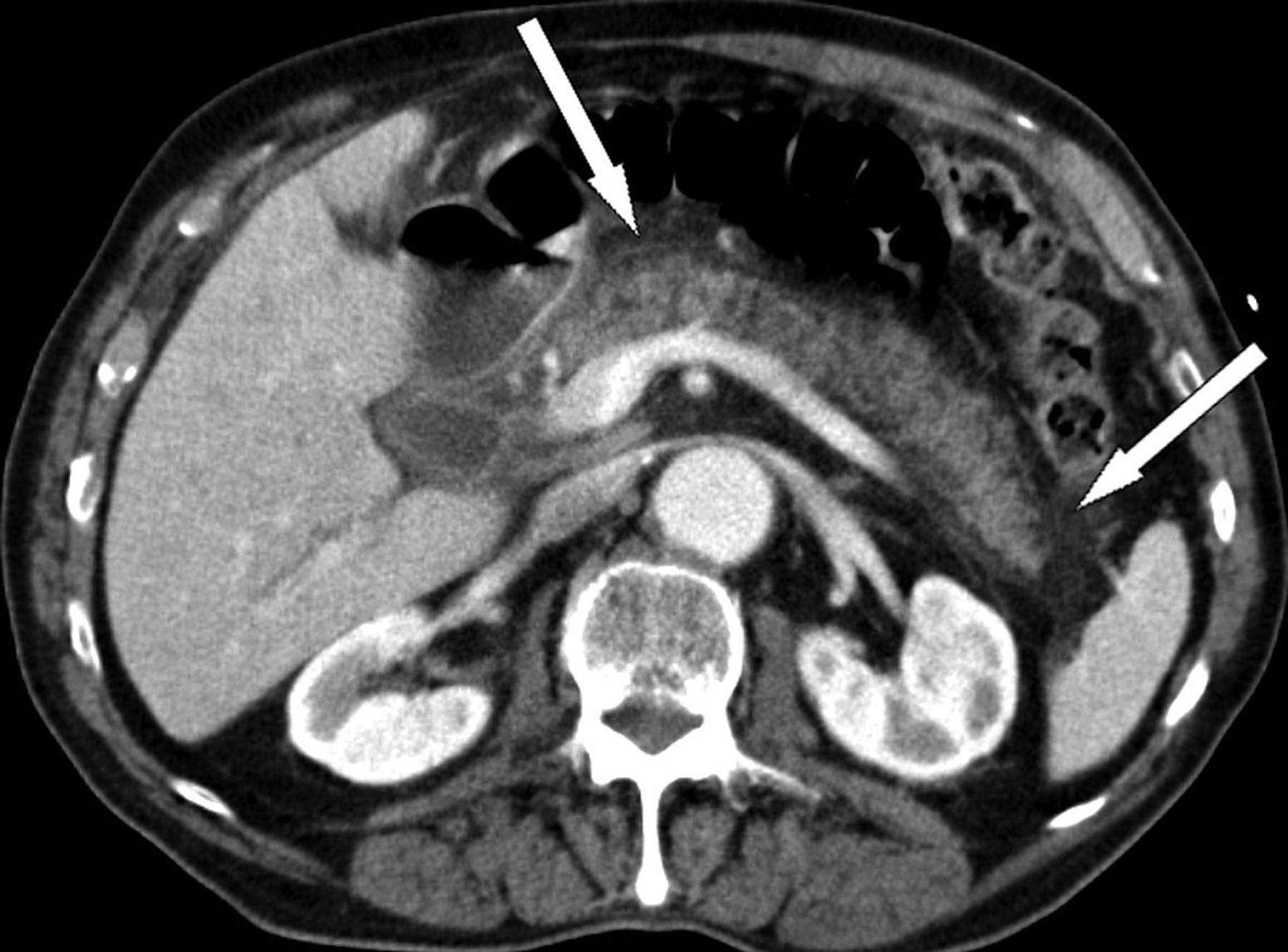
Figure: CT abdomen showed peripancreatic fat stranding and a 3.8 cm hypodense lesion in the pancreatic body.

Figure: CT abdomen revealed further Pancreatic Pseudocyst enlargement and mild diverticulitis.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Anila Mahesh indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Kishore Kumar indicated no relevant financial relationships.
Jyoti Yadav indicated no relevant financial relationships.
Jaspreet Singh indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Sunny Kumar, MD2, Anila Mahesh, MD3, Janta Devi Ukrani, MBBS, MD1, Kishore Kumar, MD4, Jyoti Yadav, MD5, Jaspreet Singh, MD6. P0113 - Ozempic-Induced Pancreatitis Leading to Recurrent Flares, Evolving Pseudocysts, and Superinfection: A Multidisciplinary Management Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
