Sunday Poster Session
Category: Biliary/Pancreas
P0112 - Acute Necrotizing Pancreatitis Following Transarterial Chemoembolization in a Patient With Metastatic Lung Cancer: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Deepak Kumar, MBBS, MD (he/him/his)
Northwell Health
Port Jefferson, NY
Presenting Author(s)
Deepak Kumar, MBBS, MD1, Lindsey Donnelly, MD2, Janta Devi Ukrani, MBBS, MD1, Muhammad Jahanzaib Khan, MBBS, MD3, Ramona Rajapakse, MD, FACG2
1Northwell Health, Port Jefferson, NY; 2Mather Hospital, Northwell Health, Port Jefferson, NY; 3Northwell at MATHER Hospital, Port Jefferson, NY
Introduction: Transarterial chemoembolization (TACE) is a key therapy for unresectable hepatic metastases but carries a rare (< 2%) risk of acute pancreatitis due to non-target embolization, chemotherapy toxicity, or ischemia. We report a rare case of acute necrotizing pancreatitis following TACE in a patient with stage IV non-small cell lung cancer (NSCLC), complicated by persistent fevers, severe pain, and imaging suggestive of hemorrhage and pseudoaneurysm.
Case Description/
Methods: A 58-year-old female with stage IV NSCLC metastatic to the liver, Neuroendocrine tumor, multiple sclerosis (MS), and chronic obstructive pulmonary disease (COPD) presented one day post-TACE with severe abdominal pain, nausea, and vomiting. Examination revealed diffuse abdominal tenderness. Laboratory findings included Hemoglobin 11.2, leukocytosis, aspartate aminotransferase 57 U/L, alanine aminotransferase 79 U/L, and lipase 1589 U/L, confirming acute pancreatitis. Initial CT showed high-density fluid around the pancreatic head and duodenum, extending to the porta hepatis, suggestive of pancreatitis and/or hemorrhage, with distal common bile duct thickening. Intravenous antibiotics and multimodal pain management were initiated, but persistent fevers and uncontrolled pain continued. Early enteral nutrition exacerbated symptoms. Repeat CT on day four revealed persistent hyperdense fluid, increased pelvic fluid, a 1.1 cm hypoattenuating pancreatic neck focus, and pancreatic head heterogeneity. Subsequent imaging identified heterogeneous hypoenhancement in the inferior pancreatic head with a 9 mm enhancing focus, suggesting early necrosis and possible pseudoaneurysm. Peripancreatic edema extended to the porta hepatis and perihepatic region. Metastatic disease remained stable. After 4–5 days of aggressive supportive care, pain improved, and clear liquids were tolerated. Magnetic resonance cholangiopancreatography confirmed necrotizing pancreatitis with organized acute necrotic collections and reduced inflammation.
Discussion: This case underscores acute necrotizing pancreatitis as a rare, life-threatening TACE complication. Early imaging, multidisciplinary collaboration, and tailored supportive care are critical for management. Clinicians must remain vigilant for vascular complications like pseudoaneurysms. Further research is needed to elucidate mechanisms and develop preventive strategies.
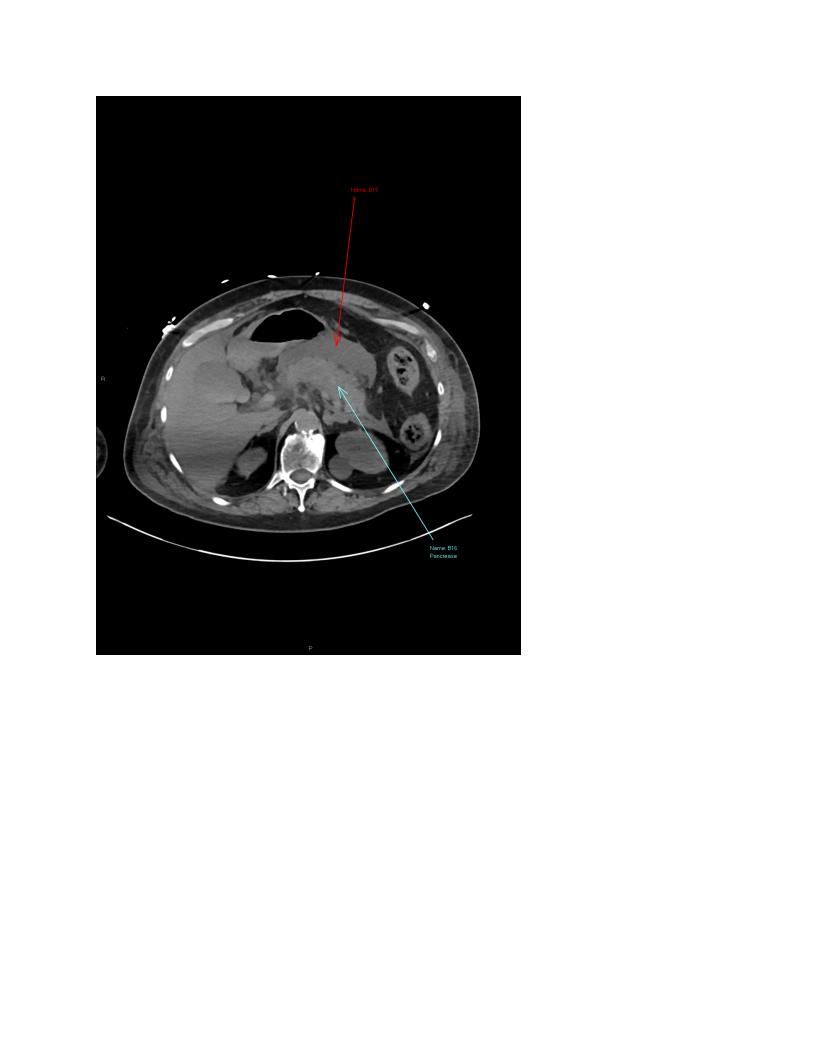
Figure: Heterogeneous hypoenhancement in the inferior pancreatic head with a 9 mm enhancing focus, suggesting early necrosis with possible pseudoaneurysm and Neuroendocrine pancreatic tumor. Peripancreatic edema extended to the porta hepatis and perihepatic region.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Lindsey Donnelly indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Lindsey Donnelly, MD2, Janta Devi Ukrani, MBBS, MD1, Muhammad Jahanzaib Khan, MBBS, MD3, Ramona Rajapakse, MD, FACG2. P0112 - Acute Necrotizing Pancreatitis Following Transarterial Chemoembolization in a Patient With Metastatic Lung Cancer: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Port Jefferson, NY; 2Mather Hospital, Northwell Health, Port Jefferson, NY; 3Northwell at MATHER Hospital, Port Jefferson, NY
Introduction: Transarterial chemoembolization (TACE) is a key therapy for unresectable hepatic metastases but carries a rare (< 2%) risk of acute pancreatitis due to non-target embolization, chemotherapy toxicity, or ischemia. We report a rare case of acute necrotizing pancreatitis following TACE in a patient with stage IV non-small cell lung cancer (NSCLC), complicated by persistent fevers, severe pain, and imaging suggestive of hemorrhage and pseudoaneurysm.
Case Description/
Methods: A 58-year-old female with stage IV NSCLC metastatic to the liver, Neuroendocrine tumor, multiple sclerosis (MS), and chronic obstructive pulmonary disease (COPD) presented one day post-TACE with severe abdominal pain, nausea, and vomiting. Examination revealed diffuse abdominal tenderness. Laboratory findings included Hemoglobin 11.2, leukocytosis, aspartate aminotransferase 57 U/L, alanine aminotransferase 79 U/L, and lipase 1589 U/L, confirming acute pancreatitis. Initial CT showed high-density fluid around the pancreatic head and duodenum, extending to the porta hepatis, suggestive of pancreatitis and/or hemorrhage, with distal common bile duct thickening. Intravenous antibiotics and multimodal pain management were initiated, but persistent fevers and uncontrolled pain continued. Early enteral nutrition exacerbated symptoms. Repeat CT on day four revealed persistent hyperdense fluid, increased pelvic fluid, a 1.1 cm hypoattenuating pancreatic neck focus, and pancreatic head heterogeneity. Subsequent imaging identified heterogeneous hypoenhancement in the inferior pancreatic head with a 9 mm enhancing focus, suggesting early necrosis and possible pseudoaneurysm. Peripancreatic edema extended to the porta hepatis and perihepatic region. Metastatic disease remained stable. After 4–5 days of aggressive supportive care, pain improved, and clear liquids were tolerated. Magnetic resonance cholangiopancreatography confirmed necrotizing pancreatitis with organized acute necrotic collections and reduced inflammation.
Discussion: This case underscores acute necrotizing pancreatitis as a rare, life-threatening TACE complication. Early imaging, multidisciplinary collaboration, and tailored supportive care are critical for management. Clinicians must remain vigilant for vascular complications like pseudoaneurysms. Further research is needed to elucidate mechanisms and develop preventive strategies.
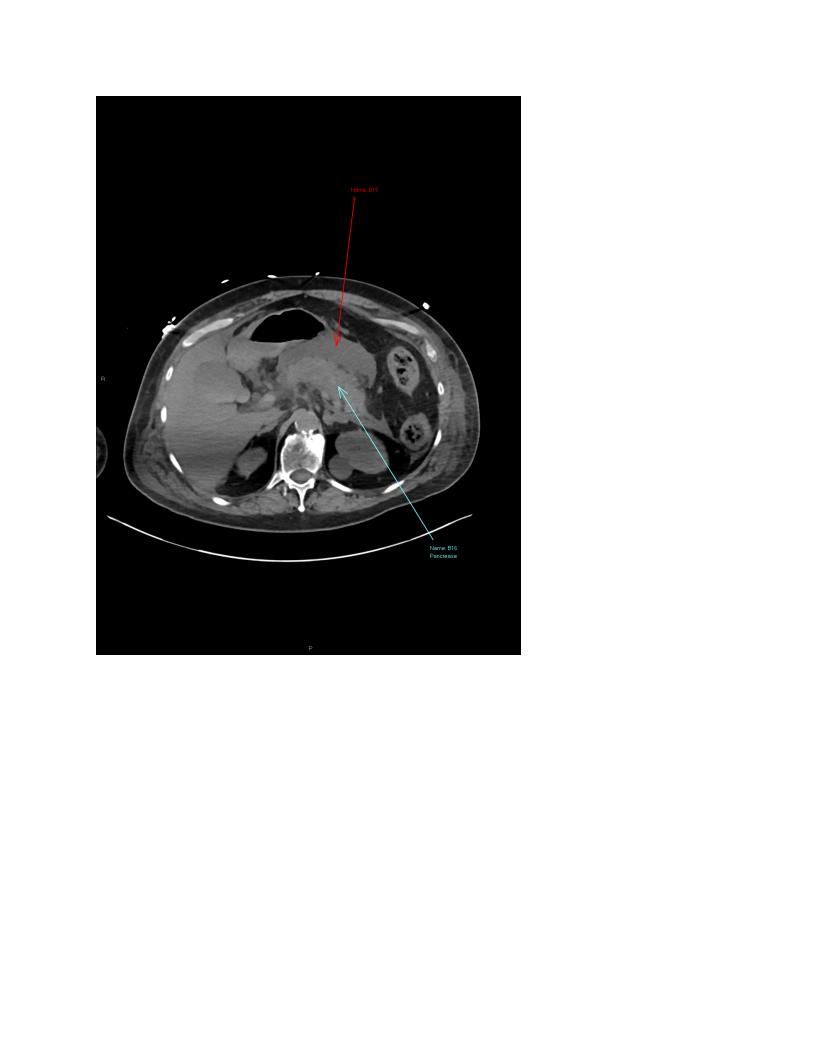
Figure: Heterogeneous hypoenhancement in the inferior pancreatic head with a 9 mm enhancing focus, suggesting early necrosis with possible pseudoaneurysm and Neuroendocrine pancreatic tumor. Peripancreatic edema extended to the porta hepatis and perihepatic region.
Disclosures:
Deepak Kumar indicated no relevant financial relationships.
Lindsey Donnelly indicated no relevant financial relationships.
Janta Devi Ukrani indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Deepak Kumar, MBBS, MD1, Lindsey Donnelly, MD2, Janta Devi Ukrani, MBBS, MD1, Muhammad Jahanzaib Khan, MBBS, MD3, Ramona Rajapakse, MD, FACG2. P0112 - Acute Necrotizing Pancreatitis Following Transarterial Chemoembolization in a Patient With Metastatic Lung Cancer: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
