Sunday Poster Session
Category: Biliary/Pancreas
P0109 - An Occult Pancreatic Neuroendocrine Tumor Diagnosed by Endoscopic Ultrasound After Normal Imaging
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tasneem Jamal Al-Din, MD
Cleveland Clinic Florida
Weston, FL
Presenting Author(s)
Tasneem Jamal Al-Din, MD, Akram Ahmad, MD, Zaid Ansari, MD, Tilak Shah, MD
Cleveland Clinic Florida, Weston, FL
Introduction: Functional pancreatic neuroendocrine tumors (PNETs) are a rare cause of chronic diarrhea, particularly vasoactive intestinal peptide-producing tumors (VIPomas). These tumors usually present with severe, symptomatic diarrhea and are often associated with widespread and aggressive metastases. However, the following case demonstrated a more indolent disease course, highlighting the variability in clinical presentation.
Case Description/
Methods: A 78-year-old male with a past medical history of hypertension and hyperlipidemia was referred for evaluation in the gastroenterology clinic for chronic diarrhea interfering with his quality of life. Two years prior, the patient had undergone a cholecystectomy, and his diarrhea was initially attributed to bile salt malabsorption. As part of the diagnostic process, bile salt binders were prescribed, but further evaluation for chronic diarrhea continued.
By the time of his clinic visit, the patient’s symptoms had resolved. However, initial lab work revealed an elevated vasoactive intestinal peptide (VIP) level of 1200 pg/mL. Additional investigations showed no abnormalities, including a complete blood count, comprehensive metabolic panel, infectious stool studies, and abdominal Magnetic Resonance Imaging (MRI) with intravenous contrast.
Given the elevated VIP level, the patient underwent a PET DOTATATE scan, which revealed an area of kerning 3 at the pancreatic uncinate process concerning for PNET (Fig1). Subsequently, endoscopic ultrasound (EUS) was performed, which identified a round hypoechoic mass measuring 7 x 5 mm in the head of the pancreas (Fig 2). Fine Needle Biopsy (FNB), which showed cells positive for CAM5.2 and synaptophysin, suspicious for PNET. The patient’s case was discussed at pancreas board, and options offered were surveillance, EUS-guided radiofrequency ablation, and surgery. Given his age and well controlled symptoms, he elected to pursue a surveillance strategy.
Discussion: The case highlights the role of EUS in identifying small PNETs, which may not be identifiable on cross-sectional imaging studies such as CT and MRI. Surveillance, ablation, and surgery are all reasonable treatment options for well-differentiated PNETs less than 2 cm in size that are causing minimal symptoms. Our case demonstrates the importance of multidisciplinary management and individualized treatment decision making.
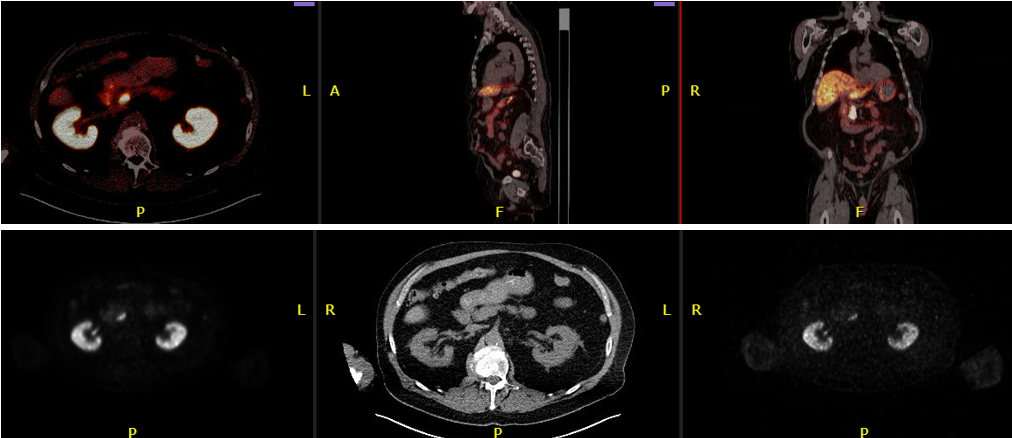
Figure: Figure 1: PET DOTATATE scan showing an area of kerning 3 at the pancreatic uncinate process.

Figure: Figure 2: Endoscopic Ultrasound Image showing anechoic-hypoechoic mass arising from a side branch of the pancreatic duct measuring 7 x 5 mm in the head of the pancreas.
Disclosures:
Tasneem Jamal Al-Din indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Tilak Shah: Steris – Consultant.
Tasneem Jamal Al-Din, MD, Akram Ahmad, MD, Zaid Ansari, MD, Tilak Shah, MD. P0109 - An Occult Pancreatic Neuroendocrine Tumor Diagnosed by Endoscopic Ultrasound After Normal Imaging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Cleveland Clinic Florida, Weston, FL
Introduction: Functional pancreatic neuroendocrine tumors (PNETs) are a rare cause of chronic diarrhea, particularly vasoactive intestinal peptide-producing tumors (VIPomas). These tumors usually present with severe, symptomatic diarrhea and are often associated with widespread and aggressive metastases. However, the following case demonstrated a more indolent disease course, highlighting the variability in clinical presentation.
Case Description/
Methods: A 78-year-old male with a past medical history of hypertension and hyperlipidemia was referred for evaluation in the gastroenterology clinic for chronic diarrhea interfering with his quality of life. Two years prior, the patient had undergone a cholecystectomy, and his diarrhea was initially attributed to bile salt malabsorption. As part of the diagnostic process, bile salt binders were prescribed, but further evaluation for chronic diarrhea continued.
By the time of his clinic visit, the patient’s symptoms had resolved. However, initial lab work revealed an elevated vasoactive intestinal peptide (VIP) level of 1200 pg/mL. Additional investigations showed no abnormalities, including a complete blood count, comprehensive metabolic panel, infectious stool studies, and abdominal Magnetic Resonance Imaging (MRI) with intravenous contrast.
Given the elevated VIP level, the patient underwent a PET DOTATATE scan, which revealed an area of kerning 3 at the pancreatic uncinate process concerning for PNET (Fig1). Subsequently, endoscopic ultrasound (EUS) was performed, which identified a round hypoechoic mass measuring 7 x 5 mm in the head of the pancreas (Fig 2). Fine Needle Biopsy (FNB), which showed cells positive for CAM5.2 and synaptophysin, suspicious for PNET. The patient’s case was discussed at pancreas board, and options offered were surveillance, EUS-guided radiofrequency ablation, and surgery. Given his age and well controlled symptoms, he elected to pursue a surveillance strategy.
Discussion: The case highlights the role of EUS in identifying small PNETs, which may not be identifiable on cross-sectional imaging studies such as CT and MRI. Surveillance, ablation, and surgery are all reasonable treatment options for well-differentiated PNETs less than 2 cm in size that are causing minimal symptoms. Our case demonstrates the importance of multidisciplinary management and individualized treatment decision making.
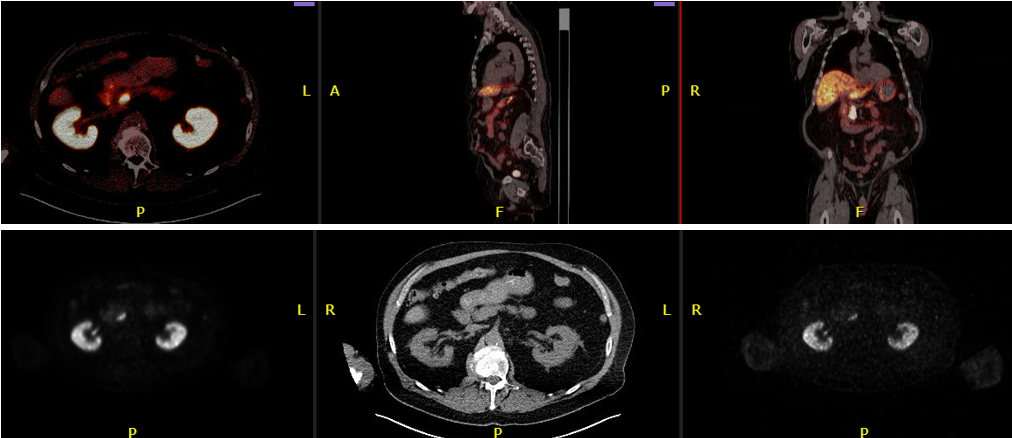
Figure: Figure 1: PET DOTATATE scan showing an area of kerning 3 at the pancreatic uncinate process.

Figure: Figure 2: Endoscopic Ultrasound Image showing anechoic-hypoechoic mass arising from a side branch of the pancreatic duct measuring 7 x 5 mm in the head of the pancreas.
Disclosures:
Tasneem Jamal Al-Din indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Tilak Shah: Steris – Consultant.
Tasneem Jamal Al-Din, MD, Akram Ahmad, MD, Zaid Ansari, MD, Tilak Shah, MD. P0109 - An Occult Pancreatic Neuroendocrine Tumor Diagnosed by Endoscopic Ultrasound After Normal Imaging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
