Sunday Poster Session
Category: Biliary/Pancreas
P0097 - Learning Curves and Bile Ducts: A Propensity-Matched Study on Trainee Involvement in Acute Cholangitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Karan J. Yagnik, MD (he/him/his)
Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University
Long Branch, NJ
Presenting Author(s)
Karan J.. Yagnik, MD1, FNU Payal, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Rahul Kumar, MD5, Avinash Nankani, MBBS6, Muhammad Ali Khan, MBBS7, Malay Rathod, MD1, Anoohya Vangala, MD1, Pranav Patel, MD8, Ben Terrany, MD1, Dhramesh Kaswala, MD1, Bradley D. Confer, DO8, Harshit S. Khara, MD9
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Mercy Catholic Medical Center, Darby, PA; 5North Central Bronx Hospital, Bronx, NY; 6Dow University of Health Sciences, Karachi, Sindh, Pakistan; 7Mayo Clinic, Phoenix, AZ; 8Geisinger Health System, Danville, PA; 9Geisinger Health System, Danville, NJ
Introduction: This study analyzed acute cholangitis (AC) outcomes in teaching hospitals, comparing July-September (new trainees) to April-June (experienced trainees). Outcomes were evaluated to determine the impact of trainee experience on patient care during these critical educational periods.
Methods: This study analyzed adult hospitalizations (age >18) with AC in U.S. teaching hospitals using the National Inpatient Sample (2016–2020). A retrospective multivariate analysis was conducted using SAS 9.4 to evaluate inpatient mortality, length of stay (LOS), total hospital charges (THC, adjusted to 2020 USD), critical care interventions (e.g., intubation, ICU admission, CVC placement), ERCP utilization (with/without intervention), and ERCP timing from admission.
Results: Total of 12360 patients were included in this analysis, out of those 6355 (~51.42%) were admitted during July-Sept and 6005 (~48.58%) were admitted during April-June across 5 years (2016-2020) period in the U.S. Median age of the patients were 73 years (IQR: 61-83) and 72 years (IQR: 61-83) for the period of July-Sept and April-June, respectively. Primary outcomes showed no difference in terms of in-patient mortality in between two groups (3.49% vs 2.95%, p=0.1061). THC was slightly higher in the April-June group ($15,492 vs $14,553) than the July-Sept group. There was significantly higher rates for ICU admissions (6.26% vs 4.83%, p=0.0009) and intubation (5.09% vs 3.75%, p=0.0006) for the patients those were managed during the months of the July-Sept than those who were managed in the April-June. But there was no difference between two groups requiring CVC line placement (1.88% vs 1.79%, p=0.7245) and ERCP utilization (85.17% vs 85.25%, p=0.8941). Analysis revealed the majority of the patients had ERCP in between 24-48 hours of admission in both the groups (51.09% vs 50.03%), than within 24 hours (25.42% vs 25.02%), and after 48 hours (23.48% vs 24.85%). However, there was no significant difference in timing between the two groups.
Discussion: Acute cholangitis has no significant difference in mortality, LOS, THC, ERCP utilization, or ERCP timing between the two groups. However, patients managed from July to September experienced higher rates of ICU admissions and intubations compared to those managed from April to June. This may indicate a lower threshold for critical interventions due to trainee inexperience, with higher life sustaining intervention rates driven by heightened patient safety measures to prevent errors.
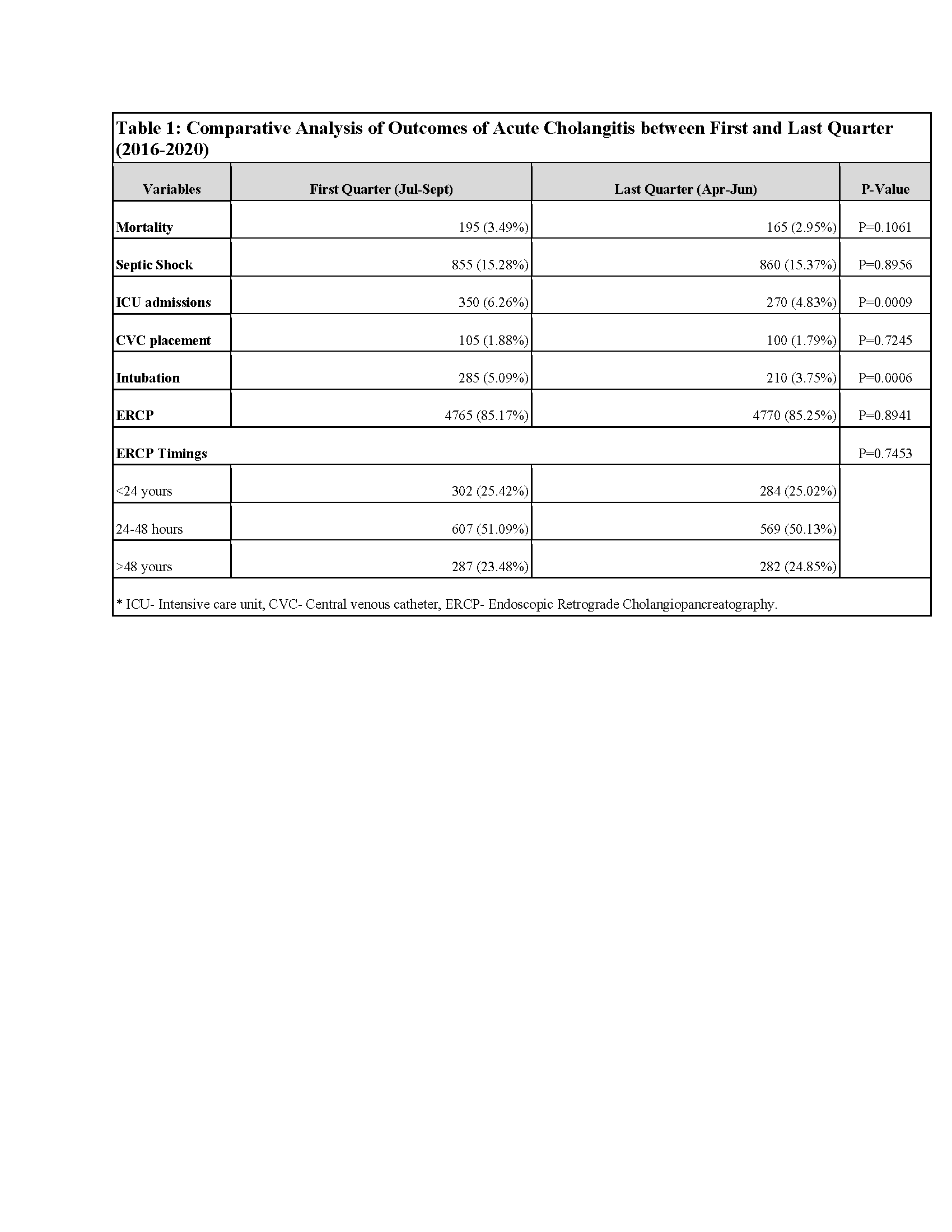
Figure: Table 1: Comparative Analysis of Outcomes of Acute Cholangitis between First and Last Quarter (2016-2020)
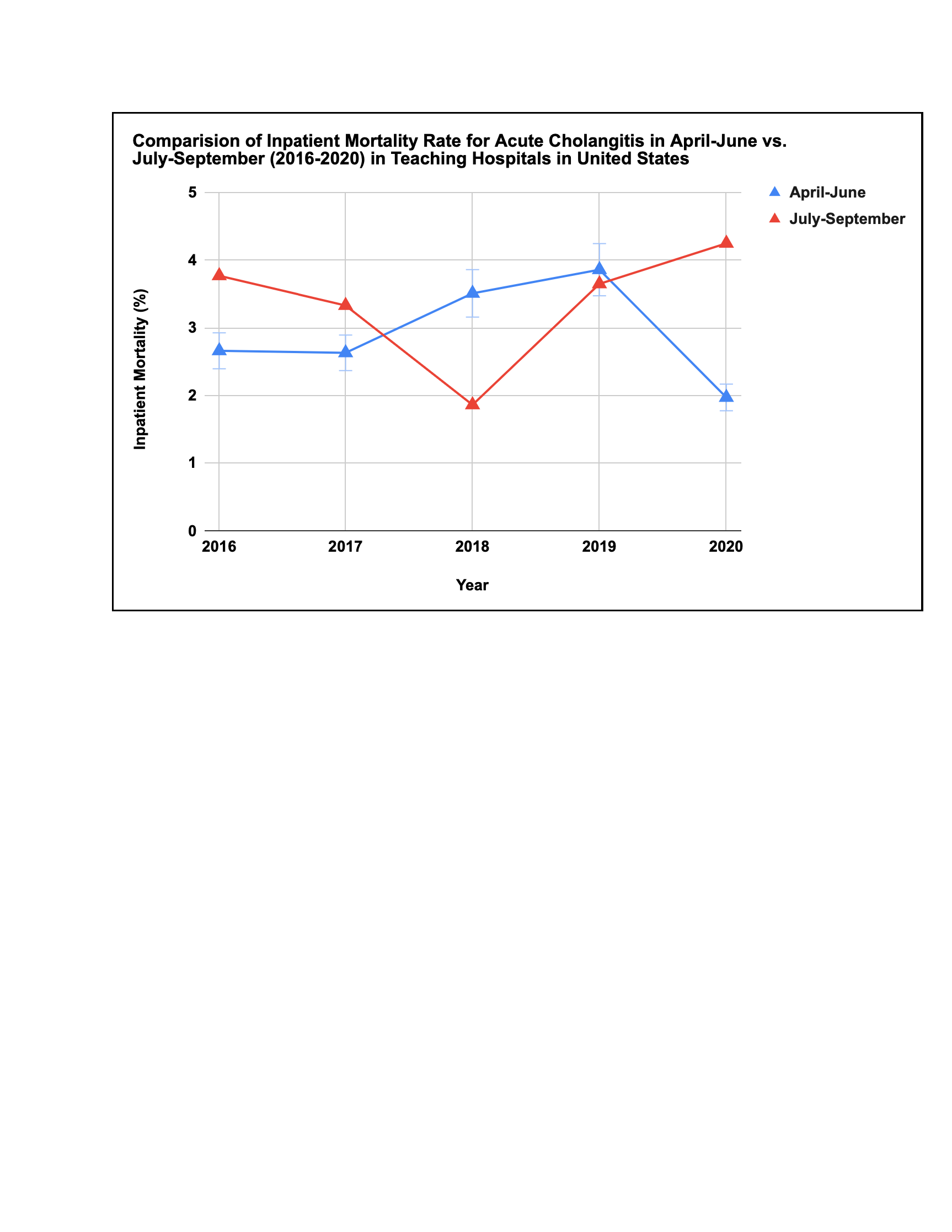
Figure: Comparision of Inpatient Mortality Rate for Acute Cholangitis in April-June vs. July-September (2016-2020) in Teaching Hospitals in United States
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
FNU Payal indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Muhammad Ali Khan indicated no relevant financial relationships.
Malay Rathod indicated no relevant financial relationships.
Anoohya Vangala indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Ben Terrany indicated no relevant financial relationships.
Dhramesh Kaswala indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, FNU Payal, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Rahul Kumar, MD5, Avinash Nankani, MBBS6, Muhammad Ali Khan, MBBS7, Malay Rathod, MD1, Anoohya Vangala, MD1, Pranav Patel, MD8, Ben Terrany, MD1, Dhramesh Kaswala, MD1, Bradley D. Confer, DO8, Harshit S. Khara, MD9. P0097 - Learning Curves and Bile Ducts: A Propensity-Matched Study on Trainee Involvement in Acute Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Mercy Catholic Medical Center, Darby, PA; 5North Central Bronx Hospital, Bronx, NY; 6Dow University of Health Sciences, Karachi, Sindh, Pakistan; 7Mayo Clinic, Phoenix, AZ; 8Geisinger Health System, Danville, PA; 9Geisinger Health System, Danville, NJ
Introduction: This study analyzed acute cholangitis (AC) outcomes in teaching hospitals, comparing July-September (new trainees) to April-June (experienced trainees). Outcomes were evaluated to determine the impact of trainee experience on patient care during these critical educational periods.
Methods: This study analyzed adult hospitalizations (age >18) with AC in U.S. teaching hospitals using the National Inpatient Sample (2016–2020). A retrospective multivariate analysis was conducted using SAS 9.4 to evaluate inpatient mortality, length of stay (LOS), total hospital charges (THC, adjusted to 2020 USD), critical care interventions (e.g., intubation, ICU admission, CVC placement), ERCP utilization (with/without intervention), and ERCP timing from admission.
Results: Total of 12360 patients were included in this analysis, out of those 6355 (~51.42%) were admitted during July-Sept and 6005 (~48.58%) were admitted during April-June across 5 years (2016-2020) period in the U.S. Median age of the patients were 73 years (IQR: 61-83) and 72 years (IQR: 61-83) for the period of July-Sept and April-June, respectively. Primary outcomes showed no difference in terms of in-patient mortality in between two groups (3.49% vs 2.95%, p=0.1061). THC was slightly higher in the April-June group ($15,492 vs $14,553) than the July-Sept group. There was significantly higher rates for ICU admissions (6.26% vs 4.83%, p=0.0009) and intubation (5.09% vs 3.75%, p=0.0006) for the patients those were managed during the months of the July-Sept than those who were managed in the April-June. But there was no difference between two groups requiring CVC line placement (1.88% vs 1.79%, p=0.7245) and ERCP utilization (85.17% vs 85.25%, p=0.8941). Analysis revealed the majority of the patients had ERCP in between 24-48 hours of admission in both the groups (51.09% vs 50.03%), than within 24 hours (25.42% vs 25.02%), and after 48 hours (23.48% vs 24.85%). However, there was no significant difference in timing between the two groups.
Discussion: Acute cholangitis has no significant difference in mortality, LOS, THC, ERCP utilization, or ERCP timing between the two groups. However, patients managed from July to September experienced higher rates of ICU admissions and intubations compared to those managed from April to June. This may indicate a lower threshold for critical interventions due to trainee inexperience, with higher life sustaining intervention rates driven by heightened patient safety measures to prevent errors.
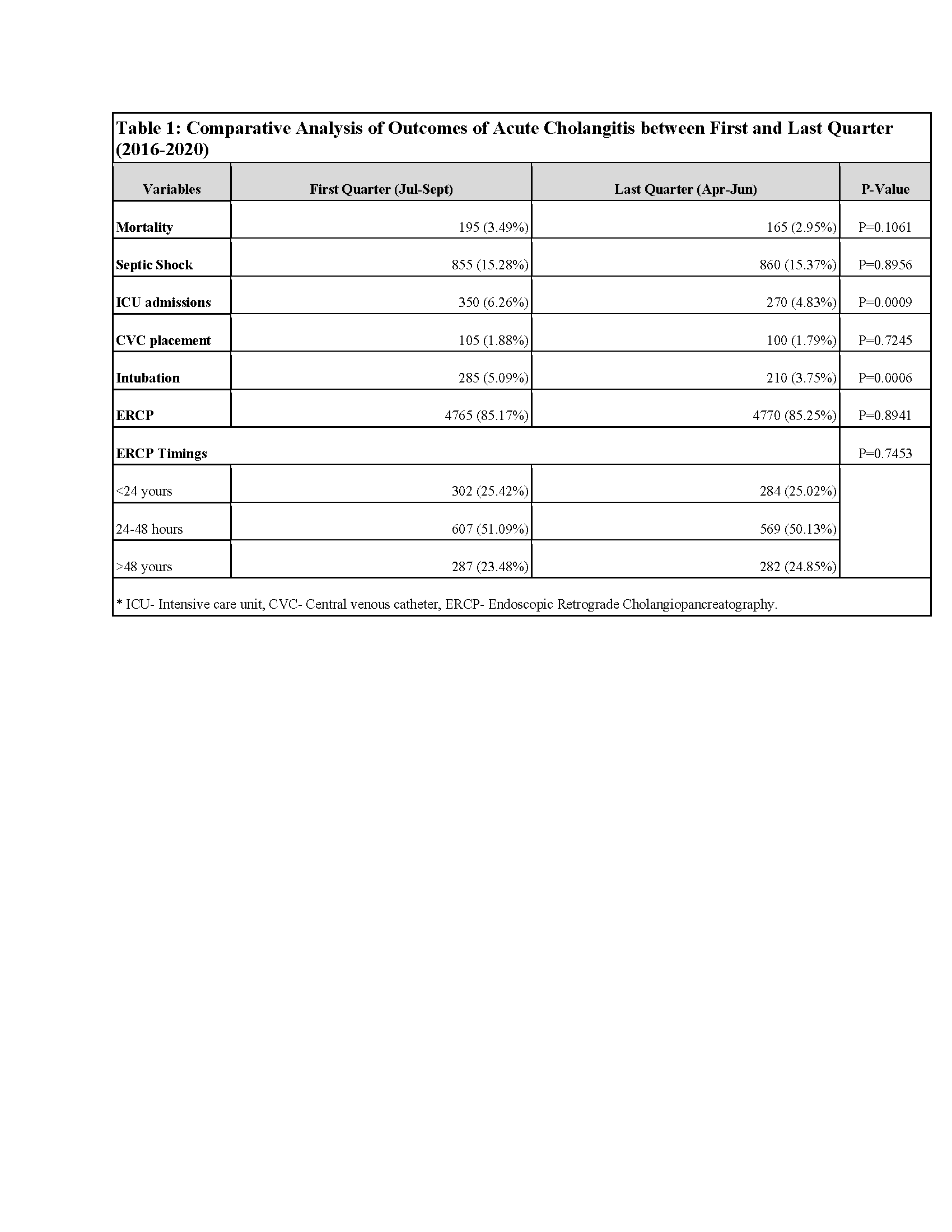
Figure: Table 1: Comparative Analysis of Outcomes of Acute Cholangitis between First and Last Quarter (2016-2020)
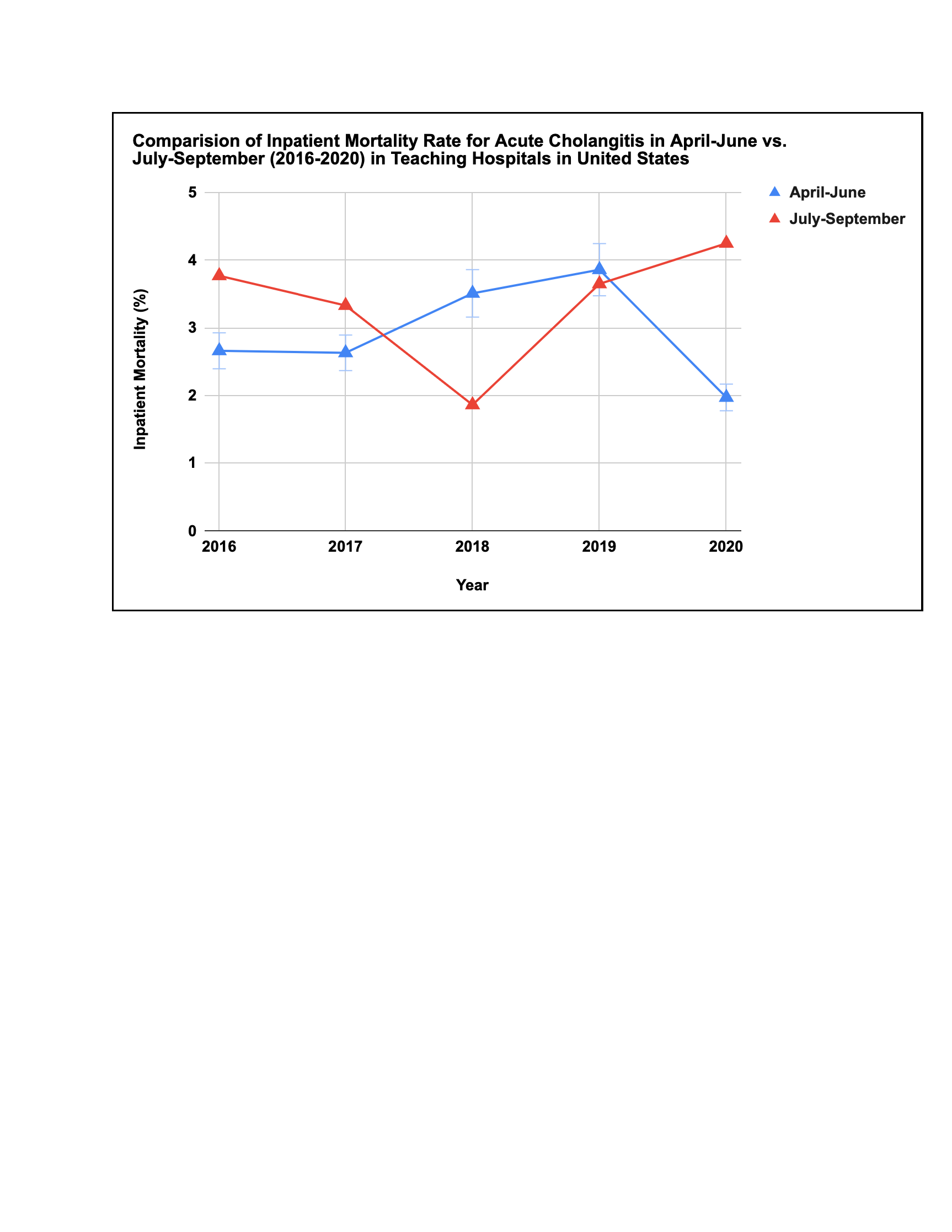
Figure: Comparision of Inpatient Mortality Rate for Acute Cholangitis in April-June vs. July-September (2016-2020) in Teaching Hospitals in United States
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
FNU Payal indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Muhammad Ali Khan indicated no relevant financial relationships.
Malay Rathod indicated no relevant financial relationships.
Anoohya Vangala indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Ben Terrany indicated no relevant financial relationships.
Dhramesh Kaswala indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, FNU Payal, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Rahul Kumar, MD5, Avinash Nankani, MBBS6, Muhammad Ali Khan, MBBS7, Malay Rathod, MD1, Anoohya Vangala, MD1, Pranav Patel, MD8, Ben Terrany, MD1, Dhramesh Kaswala, MD1, Bradley D. Confer, DO8, Harshit S. Khara, MD9. P0097 - Learning Curves and Bile Ducts: A Propensity-Matched Study on Trainee Involvement in Acute Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
