Sunday Poster Session
Category: Biliary/Pancreas
P0096 - Adverse Outcomes in Hypertriglyceridemia-Associated Acute Pancreatitis: A Propensity-Matched Cohort Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohammad Adam, MD, MSc
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Mohammad Adam, MD, MSc1, Ali Osman, MD2, Fatima Elmustafa, MBBS3, Abdelaziz Mohamed, MBBS4, Elmkdad Mohammed, MD5, Abdelhaleem Sideeg, MD6, Mohamed Ahmed, MD1, Ifrah Fatima, MD1, Mohammad Bilal, MD, FACG7, Mohamed Abdallah, MD8, Rajiv Chhabra, MD1
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Washington University, Saint Louis, MO; 3Henry Ford Warren, Warren, MI; 4One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 5The Wright Center for Graduate Medical Education, Scranton, PA; 6Virginia Mason Franciscan Health, Seattle, WA; 7University of Colorado Anschutz Medical Campus, Denver, CO; 8Corewell Health, Royal Oak, MI
Introduction: Hypertriglyceridemia-induced acute pancreatitis (HTG-AP) is the third leading cause of acute pancreatitis (AP), following gallstones and alcohol. With the growing burden of obesity, diabetes, and metabolic syndrome, HTG-AP is becoming more common. When triglyceride levels rise above 1000 mg/dL, toxic fatty acids released in the bloodstream can trigger severe pancreatic inflammation and systemic complications. Despite this, there is limited real-world data comparing outcomes between HTG-AP and other types of AP.
Methods: We used TriNetX, a global network of electronic health records, to identify adults with acute pancreatitis and either triglyceride levels ≥1000 mg/dL (HTG-AP) or < 500 mg/dL (non-HTG-AP). Patients were matched 1:1 based on age, sex, BMI, and comorbidities, yielding two cohorts of 10,034 patients each. The primary outcome was 30-day mortality. Secondary outcomes included respiratory failure, acute kidney injury (AKI), pancreatic pseudocyst formation, drainage procedures, and ED/hospital visits within six months. Baseline demographics are detailed in Table 1.
Results: HTG-AP patients were younger but experienced significantly worse outcomes. Compared to non-HTG-AP, they had higher 30-day mortality (2.2% vs. 1.5%; OR 1.49, p< 0.001), more respiratory failure (1.4% vs. 1.0%; OR 1.41, p=0.013), and greater healthcare utilization (49.0% vs. 45.3%; OR 1.16, p< 0.001). Rates of AKI (2.0% vs. 1.8%) and drainage procedures (0.3% in both) were comparable. Interestingly, pseudocyst formation was slightly more frequent in the non-HTG group (2.7% vs. 2.2%; OR 0.80, p=0.01). These outcome comparisons are illustrated in Figure 1 (Forest Plot).
Discussion: HTG-AP is associated with increased risk of mortality and complications despite affecting the younger population. Its pathophysiological profile, centered on toxic lipid metabolites, likely underlies these worse outcomes. Early recognition and aggressive triglyceride-lowering strategies are essential to reduce morbidity and mortality in this high-risk group.
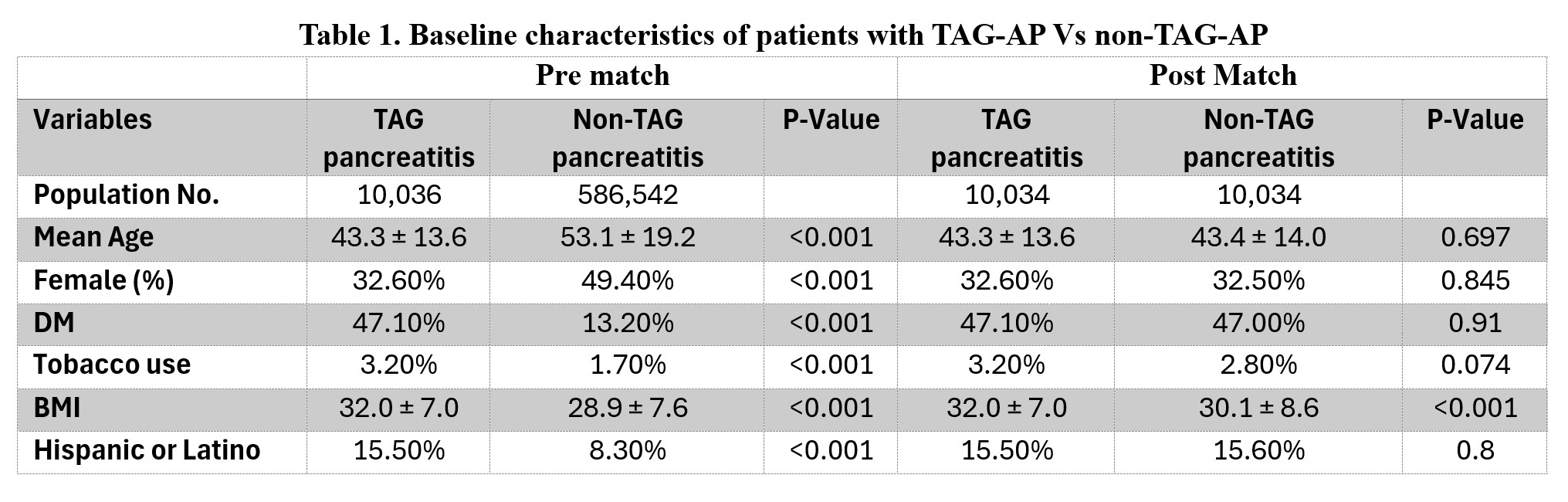
Figure: Table 1. Baseline characteristics of patients with TAG-AP Vs non-TAG-AP
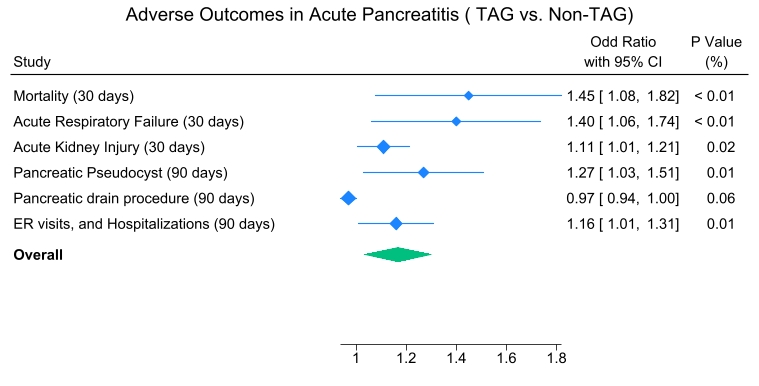
Figure: Figure 1: Forest plot illustrating odds ratios for adverse outcomes in patients with TAG-AP Vs non-TAG-AP
Disclosures:
Mohammad Adam indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Fatima Elmustafa indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Elmkdad Mohammed indicated no relevant financial relationships.
Abdelhaleem Sideeg indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Ifrah Fatima indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Mohamed Abdallah indicated no relevant financial relationships.
Rajiv Chhabra indicated no relevant financial relationships.
Mohammad Adam, MD, MSc1, Ali Osman, MD2, Fatima Elmustafa, MBBS3, Abdelaziz Mohamed, MBBS4, Elmkdad Mohammed, MD5, Abdelhaleem Sideeg, MD6, Mohamed Ahmed, MD1, Ifrah Fatima, MD1, Mohammad Bilal, MD, FACG7, Mohamed Abdallah, MD8, Rajiv Chhabra, MD1. P0096 - Adverse Outcomes in Hypertriglyceridemia-Associated Acute Pancreatitis: A Propensity-Matched Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Washington University, Saint Louis, MO; 3Henry Ford Warren, Warren, MI; 4One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 5The Wright Center for Graduate Medical Education, Scranton, PA; 6Virginia Mason Franciscan Health, Seattle, WA; 7University of Colorado Anschutz Medical Campus, Denver, CO; 8Corewell Health, Royal Oak, MI
Introduction: Hypertriglyceridemia-induced acute pancreatitis (HTG-AP) is the third leading cause of acute pancreatitis (AP), following gallstones and alcohol. With the growing burden of obesity, diabetes, and metabolic syndrome, HTG-AP is becoming more common. When triglyceride levels rise above 1000 mg/dL, toxic fatty acids released in the bloodstream can trigger severe pancreatic inflammation and systemic complications. Despite this, there is limited real-world data comparing outcomes between HTG-AP and other types of AP.
Methods: We used TriNetX, a global network of electronic health records, to identify adults with acute pancreatitis and either triglyceride levels ≥1000 mg/dL (HTG-AP) or < 500 mg/dL (non-HTG-AP). Patients were matched 1:1 based on age, sex, BMI, and comorbidities, yielding two cohorts of 10,034 patients each. The primary outcome was 30-day mortality. Secondary outcomes included respiratory failure, acute kidney injury (AKI), pancreatic pseudocyst formation, drainage procedures, and ED/hospital visits within six months. Baseline demographics are detailed in Table 1.
Results: HTG-AP patients were younger but experienced significantly worse outcomes. Compared to non-HTG-AP, they had higher 30-day mortality (2.2% vs. 1.5%; OR 1.49, p< 0.001), more respiratory failure (1.4% vs. 1.0%; OR 1.41, p=0.013), and greater healthcare utilization (49.0% vs. 45.3%; OR 1.16, p< 0.001). Rates of AKI (2.0% vs. 1.8%) and drainage procedures (0.3% in both) were comparable. Interestingly, pseudocyst formation was slightly more frequent in the non-HTG group (2.7% vs. 2.2%; OR 0.80, p=0.01). These outcome comparisons are illustrated in Figure 1 (Forest Plot).
Discussion: HTG-AP is associated with increased risk of mortality and complications despite affecting the younger population. Its pathophysiological profile, centered on toxic lipid metabolites, likely underlies these worse outcomes. Early recognition and aggressive triglyceride-lowering strategies are essential to reduce morbidity and mortality in this high-risk group.
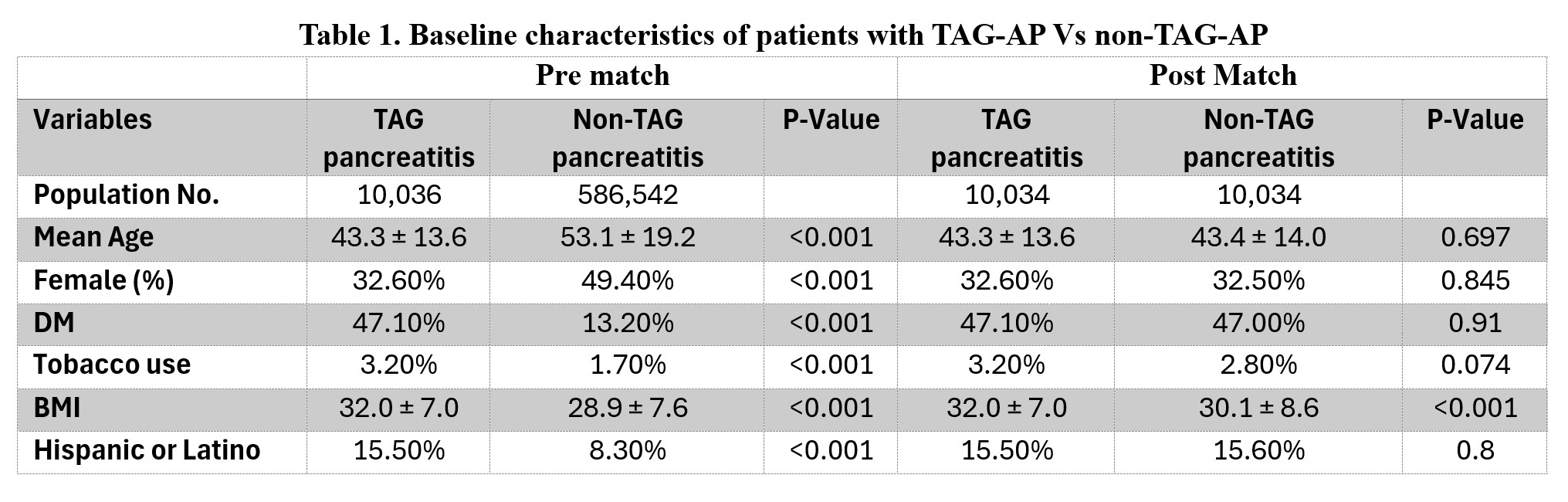
Figure: Table 1. Baseline characteristics of patients with TAG-AP Vs non-TAG-AP
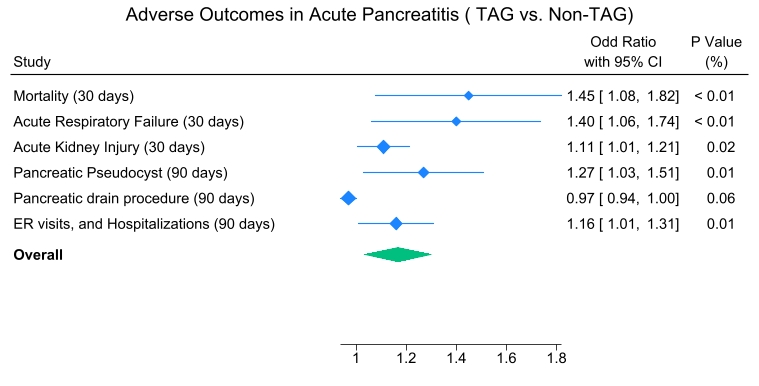
Figure: Figure 1: Forest plot illustrating odds ratios for adverse outcomes in patients with TAG-AP Vs non-TAG-AP
Disclosures:
Mohammad Adam indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Fatima Elmustafa indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Elmkdad Mohammed indicated no relevant financial relationships.
Abdelhaleem Sideeg indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Ifrah Fatima indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Mohamed Abdallah indicated no relevant financial relationships.
Rajiv Chhabra indicated no relevant financial relationships.
Mohammad Adam, MD, MSc1, Ali Osman, MD2, Fatima Elmustafa, MBBS3, Abdelaziz Mohamed, MBBS4, Elmkdad Mohammed, MD5, Abdelhaleem Sideeg, MD6, Mohamed Ahmed, MD1, Ifrah Fatima, MD1, Mohammad Bilal, MD, FACG7, Mohamed Abdallah, MD8, Rajiv Chhabra, MD1. P0096 - Adverse Outcomes in Hypertriglyceridemia-Associated Acute Pancreatitis: A Propensity-Matched Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
