Sunday Poster Session
Category: Biliary/Pancreas
P0085 - Is Obesity Associated With Worse Outcomes in ERCP?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SG
Subash Ghimire, MD
Guthrie Robert Packer Hospital, Department of Gastroenterology
Sayre, PA
Presenting Author(s)
Subash Ghimire, MD1, Amlish B. Gondal, MD2, Rasmita Budhathoki, MD3, Michelle Bernshteyn, MD1, Adishwar Rao, MD4, Tsujung Yang, MD3, Suman Sharma, MD5, Michael Georgetson, MD, FACG1, Thomas McDonald, MD1
1Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA; 2Guthrie Robert Packer Hospital, Sayre, PA, Sayre, PA; 3Guthrie Robert Packer Hospital, Sayre, PA; 4Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 5Baystate Medical Center, East Longmeadow, MA
Introduction: As prevalence of obesity has increased worldwide, the effects of this significant health issue on outcomes of common medical procedures have become even more critical. During Endoscopic retrograde cholangiopancreatography (ERCP), by altering patient’s anatomy, altering needs for positioning and sedation, limited fluoroscopic penetration, obesity may change outcomes of procedure. Current data on outcomes of ERCP on obese patients remains mixed. Our study investigates the relationship between obesity and clinical outcomes following ERCP, focusing on mortality, procedural complications, and hospitalization metrics.
Methods: This is a single center retrospective study of patients who underwent ERCP at a community teaching hospital in United States. The ERCP cohort were categorized using standard obesity classifications. We used the Kruskal-Wallis test to compare non-parametric data across all obesity groups and the Pearson Chi-Square test for categorical variables. Multivariable logistic regression model was used to predict 30-day while adjusting for comorbidities. Adjusted odds ratios (aOR) and their 95% confidence intervals (95% CI) were reported. SPSS v26 was used for statistical analysis.
Results: Among 2,741 patients who underwent ERCP, 61.9% were normal weight or overweight, while 19.7%, 9.6%, and 8.8% had Class 1, Class 2, and Class 3 obesity respectively. Increasing obesity class was associated with higher ASA score. Additionally, the prevalence of post-ERCP pancreatitis showed a similar trend (minimum with normal/overweight: 1.76% and maximum with class 3 obesity: 5.13%, p=0.03) (Table 1 & 2). No significant differences were noted in procedural duration, duration of hospitalization, perforation, and anesthesia type across obesity classes. Class 3 obesity was associated with the most significant increase in 30-day mortality (aOR 9.52, 95% CI 3.45-26.24, p< 0.05), followed by class 2 obesity (aOR 3.87, 95% CI 1.11-13.52, p=0.03). Among other comorbidities, hypertension was associated with greater odds of 30-day mortality post-ERCP (aOR 2.83, 95% CI 1.08-7.97, p=0.04).
Discussion: Class 2 and Class 3 obesity are independent predictors of post-ERCP pancreatitis and increased 30-day mortality post-ERCP. These findings highlight the need for careful risk assessment, procedural planning and post procedure monitoring in these patients.
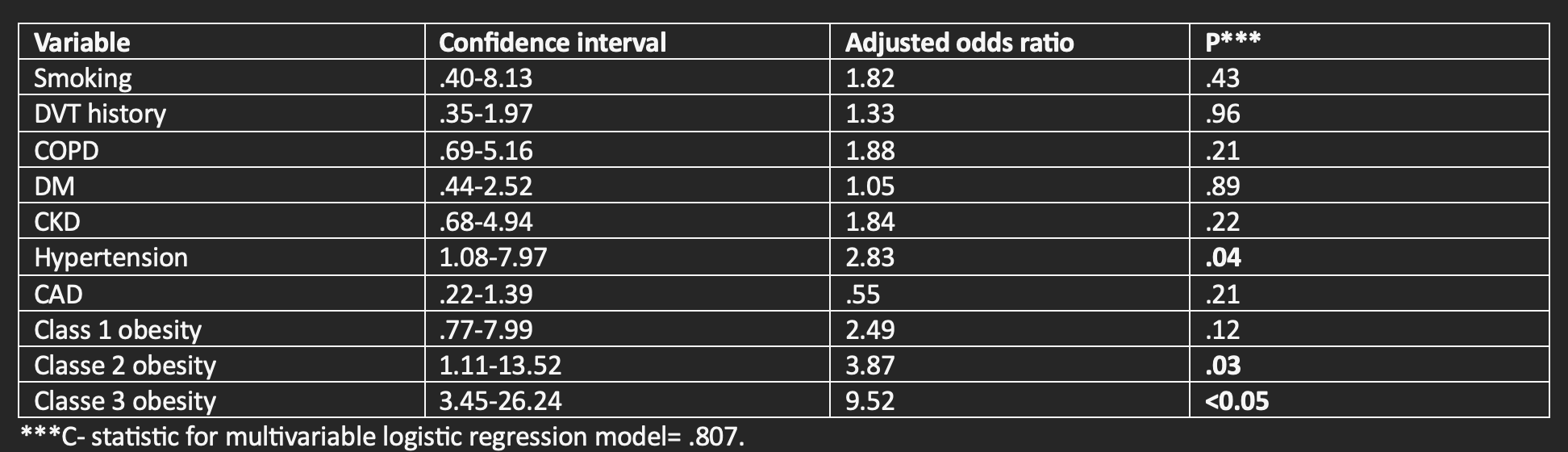
Figure: Table 1: Distribution of characteristics of patients undergoing ERCP with obesity
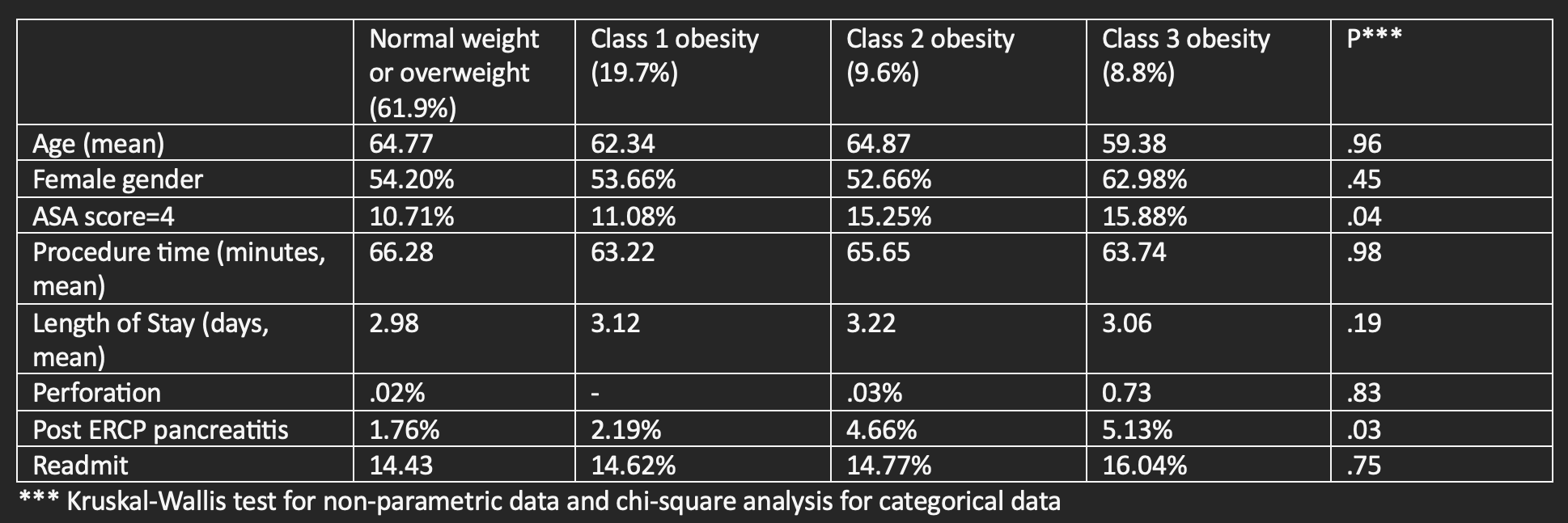
Figure: Table 2: Impact of Obesity in Relation to Comorbidities on Mortality within 30 days after ERCP
Disclosures:
Subash Ghimire indicated no relevant financial relationships.
Amlish Gondal indicated no relevant financial relationships.
Rasmita Budhathoki indicated no relevant financial relationships.
Michelle Bernshteyn indicated no relevant financial relationships.
Adishwar Rao indicated no relevant financial relationships.
Tsujung Yang indicated no relevant financial relationships.
Suman Sharma indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Thomas McDonald indicated no relevant financial relationships.
Subash Ghimire, MD1, Amlish B. Gondal, MD2, Rasmita Budhathoki, MD3, Michelle Bernshteyn, MD1, Adishwar Rao, MD4, Tsujung Yang, MD3, Suman Sharma, MD5, Michael Georgetson, MD, FACG1, Thomas McDonald, MD1. P0085 - Is Obesity Associated With Worse Outcomes in ERCP?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA; 2Guthrie Robert Packer Hospital, Sayre, PA, Sayre, PA; 3Guthrie Robert Packer Hospital, Sayre, PA; 4Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 5Baystate Medical Center, East Longmeadow, MA
Introduction: As prevalence of obesity has increased worldwide, the effects of this significant health issue on outcomes of common medical procedures have become even more critical. During Endoscopic retrograde cholangiopancreatography (ERCP), by altering patient’s anatomy, altering needs for positioning and sedation, limited fluoroscopic penetration, obesity may change outcomes of procedure. Current data on outcomes of ERCP on obese patients remains mixed. Our study investigates the relationship between obesity and clinical outcomes following ERCP, focusing on mortality, procedural complications, and hospitalization metrics.
Methods: This is a single center retrospective study of patients who underwent ERCP at a community teaching hospital in United States. The ERCP cohort were categorized using standard obesity classifications. We used the Kruskal-Wallis test to compare non-parametric data across all obesity groups and the Pearson Chi-Square test for categorical variables. Multivariable logistic regression model was used to predict 30-day while adjusting for comorbidities. Adjusted odds ratios (aOR) and their 95% confidence intervals (95% CI) were reported. SPSS v26 was used for statistical analysis.
Results: Among 2,741 patients who underwent ERCP, 61.9% were normal weight or overweight, while 19.7%, 9.6%, and 8.8% had Class 1, Class 2, and Class 3 obesity respectively. Increasing obesity class was associated with higher ASA score. Additionally, the prevalence of post-ERCP pancreatitis showed a similar trend (minimum with normal/overweight: 1.76% and maximum with class 3 obesity: 5.13%, p=0.03) (Table 1 & 2). No significant differences were noted in procedural duration, duration of hospitalization, perforation, and anesthesia type across obesity classes. Class 3 obesity was associated with the most significant increase in 30-day mortality (aOR 9.52, 95% CI 3.45-26.24, p< 0.05), followed by class 2 obesity (aOR 3.87, 95% CI 1.11-13.52, p=0.03). Among other comorbidities, hypertension was associated with greater odds of 30-day mortality post-ERCP (aOR 2.83, 95% CI 1.08-7.97, p=0.04).
Discussion: Class 2 and Class 3 obesity are independent predictors of post-ERCP pancreatitis and increased 30-day mortality post-ERCP. These findings highlight the need for careful risk assessment, procedural planning and post procedure monitoring in these patients.
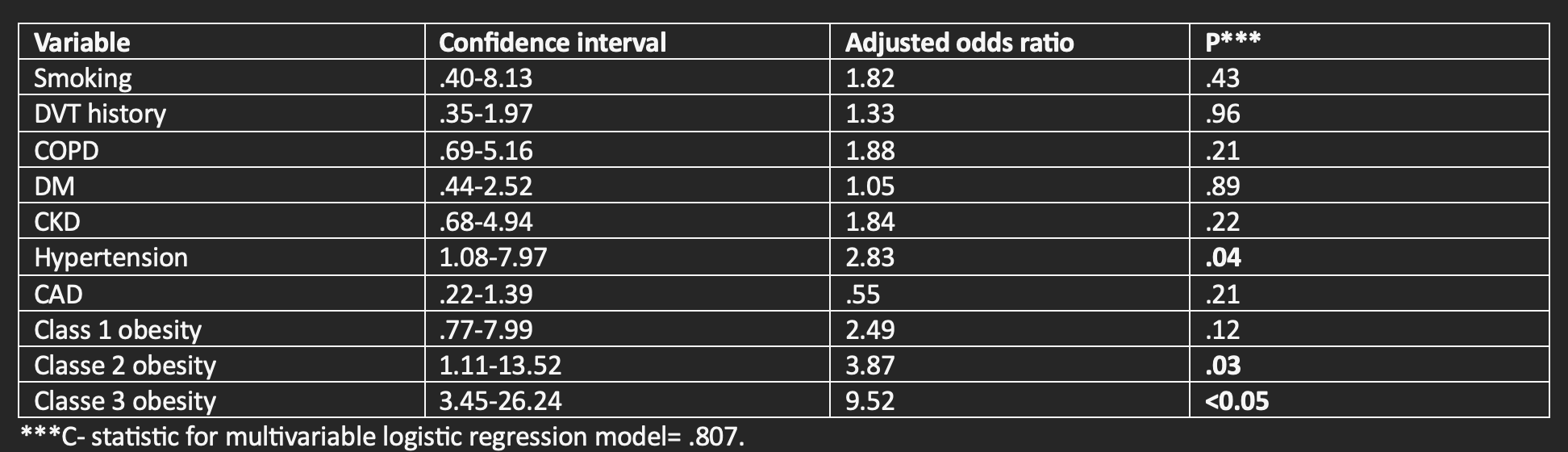
Figure: Table 1: Distribution of characteristics of patients undergoing ERCP with obesity
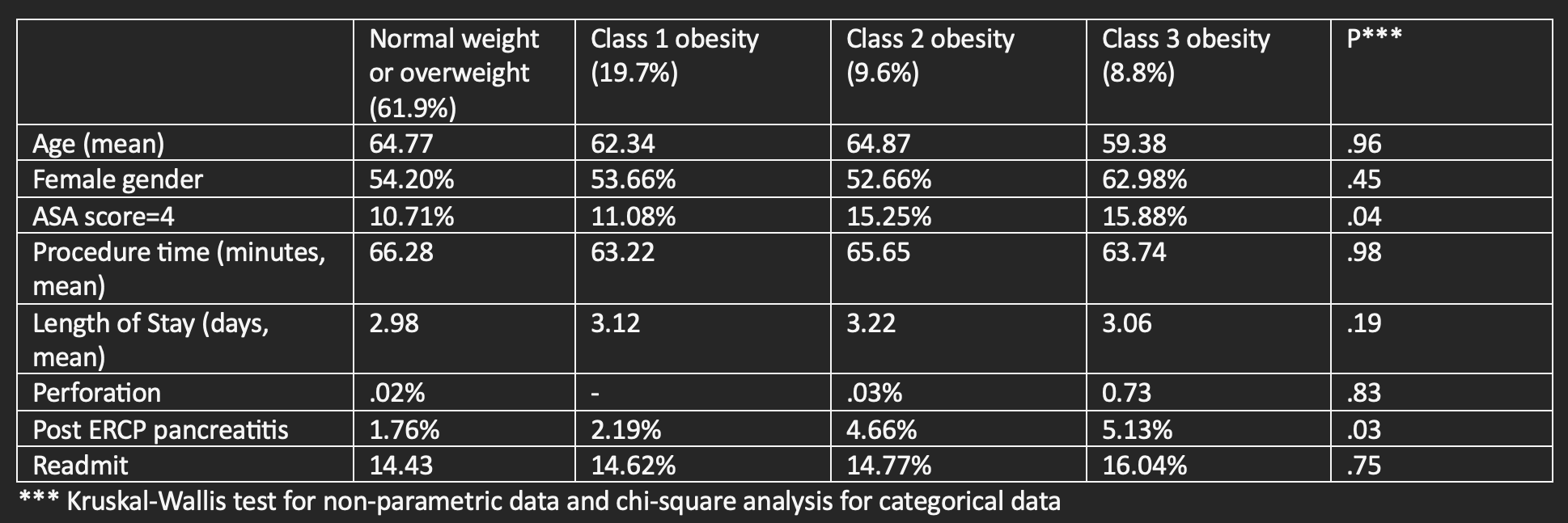
Figure: Table 2: Impact of Obesity in Relation to Comorbidities on Mortality within 30 days after ERCP
Disclosures:
Subash Ghimire indicated no relevant financial relationships.
Amlish Gondal indicated no relevant financial relationships.
Rasmita Budhathoki indicated no relevant financial relationships.
Michelle Bernshteyn indicated no relevant financial relationships.
Adishwar Rao indicated no relevant financial relationships.
Tsujung Yang indicated no relevant financial relationships.
Suman Sharma indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Thomas McDonald indicated no relevant financial relationships.
Subash Ghimire, MD1, Amlish B. Gondal, MD2, Rasmita Budhathoki, MD3, Michelle Bernshteyn, MD1, Adishwar Rao, MD4, Tsujung Yang, MD3, Suman Sharma, MD5, Michael Georgetson, MD, FACG1, Thomas McDonald, MD1. P0085 - Is Obesity Associated With Worse Outcomes in ERCP?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
