Sunday Poster Session
Category: Biliary/Pancreas
P0084 - Machine Learning and Deep Learning Models for Predicting Acute Kidney Injury in Acute Pancreatitis: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Prakhar Bajpai, MBBS (he/him/his)
Jawaharlal Nehru Medical College, Belagavi, India
Dehradun, Uttarakhand, India
Presenting Author(s)
Prakhar Bajpai, MBBS1, Bhavana Baraskar, MD2, Karan Gherwada, MBBS3, Thiruvikram Sivakumar, MBBS4, Suprada Vinyak, MD5, Saiyeeda Tahrima, MBBS6, Praveena Duggi, MBBS7, Niraj Balakrishnan, MBBS4, Rupak Desai, MBBS8
1Jawaharlal Nehru Medical College, Belagavi, India, Belagavi, Karnataka, India; 2Mary Washington Healthcare, Fredericksburg, VA; 3P. D. Hinduja Hospital and Medical Research Centre, Mumbai, Maharashtra, India; 4SRM Medical College Hospital and Research Centre, Kattankulathur, Tamil Nadu, India; 5Emory University Hospital, Atlanta, GA; 6Rajshahi Medical College Hospital, Rajshahi, Rajshahi, Bangladesh; 7A.C.S.R Government Medical College, Nellore, Andhra Pradesh, India; 8Independent Outcomes Researcher, Atlanta, GA
Introduction: Acute kidney injury (AKI) is a severe complication of acute pancreatitis (AP), with mortality reaching up to 75%. Traditional scoring systems often underperform due to AP’s heterogeneity and AKI’s multifactorial nature. Artificial intelligence (AI) methods, including machine learning (ML) and deep learning (DL), show promise for early AKI prediction by capturing non-linear clinical patterns; however, their application in AP remains limited. This systematic review and meta-analysis assesses current AI-based models for AKI prediction in AP, identifies gaps in validation and implementation, and guides future research and clinical integration.
Methods: We searched PubMed and Google Scholar through May 2025, supplemented by snowballing, to identify studies that developed or validated ML/DL models for predicting AKI in AP using area under the curve (AUC) as the performance metric. Seven retrospective studies using clinical or public datasets (e.g., MIMIC) were included. Models were categorised as: (1) linear (e.g., LR, LASSO), (2) tree-based/ensemble (e.g., RF, XGBoost), (3) neural/deep learning (e.g., ANN, DL), and (4) kernel/probabilistic (e.g., SVM). Extracted data included predictors, validation methods, and AUCs. Pooled AUCs were estimated using a random-effects model; heterogeneity was assessed via I², and robustness was evaluated with leave-one-out analysis.
Results: Across seven studies (n=4,549), ML/DL models outperformed logistic regression (LR) in predicting AKI in AP, with pooled AUCs of 0.83 (95% CI: 0.82–0.85; I² = 65.9%) vs. 0.80 (95% CI: 0.78–0.83; I² = 54.5%). Tree-based models achieved the highest subgroup performance (AUC=0.86), followed by kernel/probabilistic (0.84) and neural/deep learning models (0.82). Forest plots demonstrated consistency with low heterogeneity, and leave-one-out analysis confirmed robustness (AUC range: 0.82–0.85). Common predictors included creatinine, CRP, IL-6, SOFA, APACHE II scores, age, and fluid balance. Few studies incorporated external validation or interpretability tools.
Discussion: ML/DL models, particularly tree-based models and SVM, surpass LR in predicting AKI in AP, with a pooled AUC of 0.83, by effectively handling complex data for early risk stratification. However, limited interpretability (e.g., lacking SHAP), inconsistent predictors, and scarce external validation hinder clinical adoption. Future research must enhance model transparency, validation, and clinical integration to improve early risk prediction and patient outcomes.
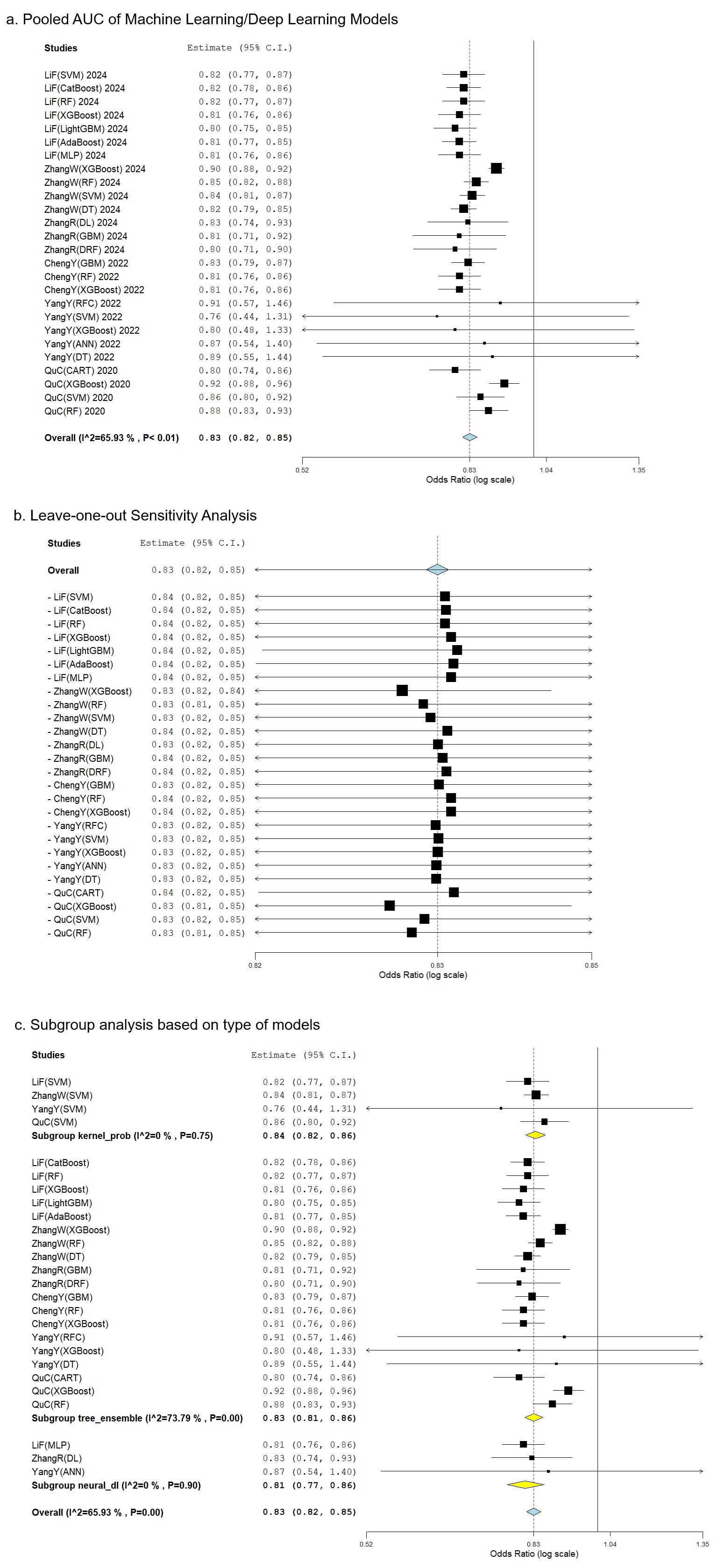
Figure: Machine Learning & Deep Learning Models for Predicting Acute Kidney Injury in Acute Pancreatitis: A Systematic Review and Meta-analysis. (a) Pooled AUC of Machine Learning/Deep Learning Models. (b) Leave-one-out Sensitivity Analysis. (c) Subgroup analysis based on the type of models.
Disclosures:
Prakhar Bajpai indicated no relevant financial relationships.
Bhavana Baraskar indicated no relevant financial relationships.
Karan Gherwada indicated no relevant financial relationships.
Thiruvikram Sivakumar indicated no relevant financial relationships.
Suprada Vinyak indicated no relevant financial relationships.
Saiyeeda Tahrima indicated no relevant financial relationships.
Praveena Duggi indicated no relevant financial relationships.
Niraj Balakrishnan indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Prakhar Bajpai, MBBS1, Bhavana Baraskar, MD2, Karan Gherwada, MBBS3, Thiruvikram Sivakumar, MBBS4, Suprada Vinyak, MD5, Saiyeeda Tahrima, MBBS6, Praveena Duggi, MBBS7, Niraj Balakrishnan, MBBS4, Rupak Desai, MBBS8. P0084 - Machine Learning and Deep Learning Models for Predicting Acute Kidney Injury in Acute Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jawaharlal Nehru Medical College, Belagavi, India, Belagavi, Karnataka, India; 2Mary Washington Healthcare, Fredericksburg, VA; 3P. D. Hinduja Hospital and Medical Research Centre, Mumbai, Maharashtra, India; 4SRM Medical College Hospital and Research Centre, Kattankulathur, Tamil Nadu, India; 5Emory University Hospital, Atlanta, GA; 6Rajshahi Medical College Hospital, Rajshahi, Rajshahi, Bangladesh; 7A.C.S.R Government Medical College, Nellore, Andhra Pradesh, India; 8Independent Outcomes Researcher, Atlanta, GA
Introduction: Acute kidney injury (AKI) is a severe complication of acute pancreatitis (AP), with mortality reaching up to 75%. Traditional scoring systems often underperform due to AP’s heterogeneity and AKI’s multifactorial nature. Artificial intelligence (AI) methods, including machine learning (ML) and deep learning (DL), show promise for early AKI prediction by capturing non-linear clinical patterns; however, their application in AP remains limited. This systematic review and meta-analysis assesses current AI-based models for AKI prediction in AP, identifies gaps in validation and implementation, and guides future research and clinical integration.
Methods: We searched PubMed and Google Scholar through May 2025, supplemented by snowballing, to identify studies that developed or validated ML/DL models for predicting AKI in AP using area under the curve (AUC) as the performance metric. Seven retrospective studies using clinical or public datasets (e.g., MIMIC) were included. Models were categorised as: (1) linear (e.g., LR, LASSO), (2) tree-based/ensemble (e.g., RF, XGBoost), (3) neural/deep learning (e.g., ANN, DL), and (4) kernel/probabilistic (e.g., SVM). Extracted data included predictors, validation methods, and AUCs. Pooled AUCs were estimated using a random-effects model; heterogeneity was assessed via I², and robustness was evaluated with leave-one-out analysis.
Results: Across seven studies (n=4,549), ML/DL models outperformed logistic regression (LR) in predicting AKI in AP, with pooled AUCs of 0.83 (95% CI: 0.82–0.85; I² = 65.9%) vs. 0.80 (95% CI: 0.78–0.83; I² = 54.5%). Tree-based models achieved the highest subgroup performance (AUC=0.86), followed by kernel/probabilistic (0.84) and neural/deep learning models (0.82). Forest plots demonstrated consistency with low heterogeneity, and leave-one-out analysis confirmed robustness (AUC range: 0.82–0.85). Common predictors included creatinine, CRP, IL-6, SOFA, APACHE II scores, age, and fluid balance. Few studies incorporated external validation or interpretability tools.
Discussion: ML/DL models, particularly tree-based models and SVM, surpass LR in predicting AKI in AP, with a pooled AUC of 0.83, by effectively handling complex data for early risk stratification. However, limited interpretability (e.g., lacking SHAP), inconsistent predictors, and scarce external validation hinder clinical adoption. Future research must enhance model transparency, validation, and clinical integration to improve early risk prediction and patient outcomes.
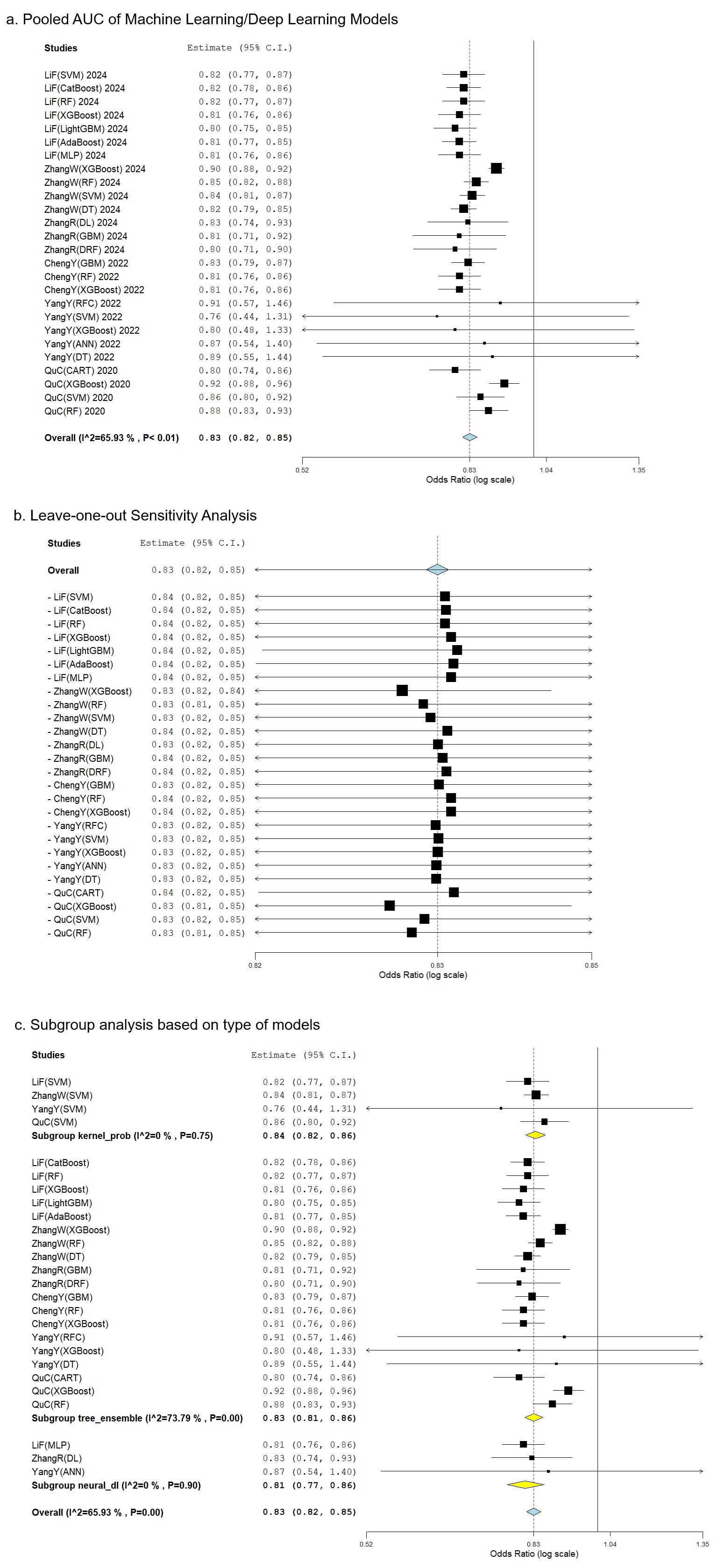
Figure: Machine Learning & Deep Learning Models for Predicting Acute Kidney Injury in Acute Pancreatitis: A Systematic Review and Meta-analysis. (a) Pooled AUC of Machine Learning/Deep Learning Models. (b) Leave-one-out Sensitivity Analysis. (c) Subgroup analysis based on the type of models.
Disclosures:
Prakhar Bajpai indicated no relevant financial relationships.
Bhavana Baraskar indicated no relevant financial relationships.
Karan Gherwada indicated no relevant financial relationships.
Thiruvikram Sivakumar indicated no relevant financial relationships.
Suprada Vinyak indicated no relevant financial relationships.
Saiyeeda Tahrima indicated no relevant financial relationships.
Praveena Duggi indicated no relevant financial relationships.
Niraj Balakrishnan indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Prakhar Bajpai, MBBS1, Bhavana Baraskar, MD2, Karan Gherwada, MBBS3, Thiruvikram Sivakumar, MBBS4, Suprada Vinyak, MD5, Saiyeeda Tahrima, MBBS6, Praveena Duggi, MBBS7, Niraj Balakrishnan, MBBS4, Rupak Desai, MBBS8. P0084 - Machine Learning and Deep Learning Models for Predicting Acute Kidney Injury in Acute Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

