Sunday Poster Session
Category: Biliary/Pancreas
P0078 - An Evaluation of Racial Disparities in Outcomes of Post Endoscopic Retrograde Cholangiopancreatography Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AG
Amlish Gondal, MD
Guthrie Robert Packer Hospital, Department of Internal Medicine
Sayre, PA
Presenting Author(s)
Amlish Gondal, MD1, Ali Jaan, MD2, Raja Chandra Chakinala, MD3, Subash Ghimire, MD3, Ezza Bashir, MBBS4, Michael Georgetson, MD, FACG3
1Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 2Rochester Regional Health, Rochester, NY; 3Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA; 4Akhtar Saeed medical College, Lahore, Punjab, Pakistan
Introduction: Racial minorities have a higher burden of exocrine pancreatic disease. Prior epidemiological studies indicate a rise in inpatient mortality following an index endoscopic retrograde cholangiopancreatography (ERCP) for African American and Hispanic patients. Data on outcomes of post-ERCP pancreatitis (PEP) remains sparse. This study aims to analyze the association of race with outcomes following post-ERCP pancreatitis.
Methods: Using International Classification of Diseases-10 (ICD-10) codes, we sampled adult patients with PEP from the National Inpatient Sample 2020. Local and systemic complications from PEP were compared among races. Proportions were analyzed using Fisher’s exact test, and multivariate logistic regression was performed, adjusting for age, gender, comorbidities, procedure volume, and patient and hospital factors. We used Stata, version 14.2, to perform analyses considering 2-sided P< 0.05 as statistically significant.
Results: A total 8315 patients with PEP were identified in the NIS; 11.9% were African American, 15.9% were Hispanic. Adjusted odds for local complications were similar in all 3 major racial groups (p >0.05, Table 1). African American were more likely to develop intestinal obstruction following PEP (adjusted odds ratio (aOR) 2.05, p=0.02) and kidney injury (aOR 1.95 p=0.001). Hispanic patients were more likely to develop sepsis (aOR 1.61 p=0.03). Mortality was similar among all groups.
Discussion: Racial minorities demonstrated comparable mortality rates following post-ERCP pancreatitis (PEP), differing from earlier studies that reported increased mortality across all etiologies of pancreatitis. This discrepancy may be attributed to the standardized, protocol-driven care often employed in PEP cases, possibly due to greater involvement of gastroenterology specialists. Notably, African American patients exhibited higher odds of gastrointestinal obstruction and acute kidney injury, while Hispanic patients had increased odds of developing sepsis.
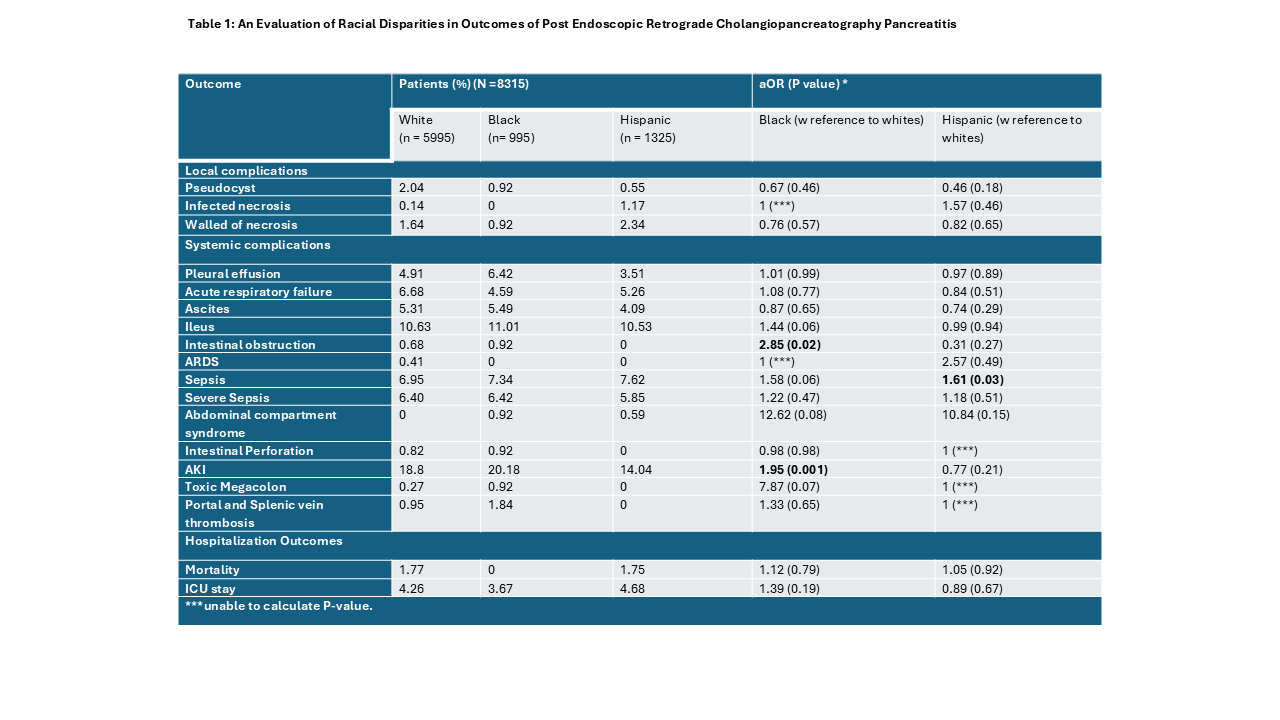
Figure: Table 1
Disclosures:
Amlish Gondal indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Raja Chandra Chakinala indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Ezza Bashir indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Amlish Gondal, MD1, Ali Jaan, MD2, Raja Chandra Chakinala, MD3, Subash Ghimire, MD3, Ezza Bashir, MBBS4, Michael Georgetson, MD, FACG3. P0078 - An Evaluation of Racial Disparities in Outcomes of Post Endoscopic Retrograde Cholangiopancreatography Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 2Rochester Regional Health, Rochester, NY; 3Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA; 4Akhtar Saeed medical College, Lahore, Punjab, Pakistan
Introduction: Racial minorities have a higher burden of exocrine pancreatic disease. Prior epidemiological studies indicate a rise in inpatient mortality following an index endoscopic retrograde cholangiopancreatography (ERCP) for African American and Hispanic patients. Data on outcomes of post-ERCP pancreatitis (PEP) remains sparse. This study aims to analyze the association of race with outcomes following post-ERCP pancreatitis.
Methods: Using International Classification of Diseases-10 (ICD-10) codes, we sampled adult patients with PEP from the National Inpatient Sample 2020. Local and systemic complications from PEP were compared among races. Proportions were analyzed using Fisher’s exact test, and multivariate logistic regression was performed, adjusting for age, gender, comorbidities, procedure volume, and patient and hospital factors. We used Stata, version 14.2, to perform analyses considering 2-sided P< 0.05 as statistically significant.
Results: A total 8315 patients with PEP were identified in the NIS; 11.9% were African American, 15.9% were Hispanic. Adjusted odds for local complications were similar in all 3 major racial groups (p >0.05, Table 1). African American were more likely to develop intestinal obstruction following PEP (adjusted odds ratio (aOR) 2.05, p=0.02) and kidney injury (aOR 1.95 p=0.001). Hispanic patients were more likely to develop sepsis (aOR 1.61 p=0.03). Mortality was similar among all groups.
Discussion: Racial minorities demonstrated comparable mortality rates following post-ERCP pancreatitis (PEP), differing from earlier studies that reported increased mortality across all etiologies of pancreatitis. This discrepancy may be attributed to the standardized, protocol-driven care often employed in PEP cases, possibly due to greater involvement of gastroenterology specialists. Notably, African American patients exhibited higher odds of gastrointestinal obstruction and acute kidney injury, while Hispanic patients had increased odds of developing sepsis.
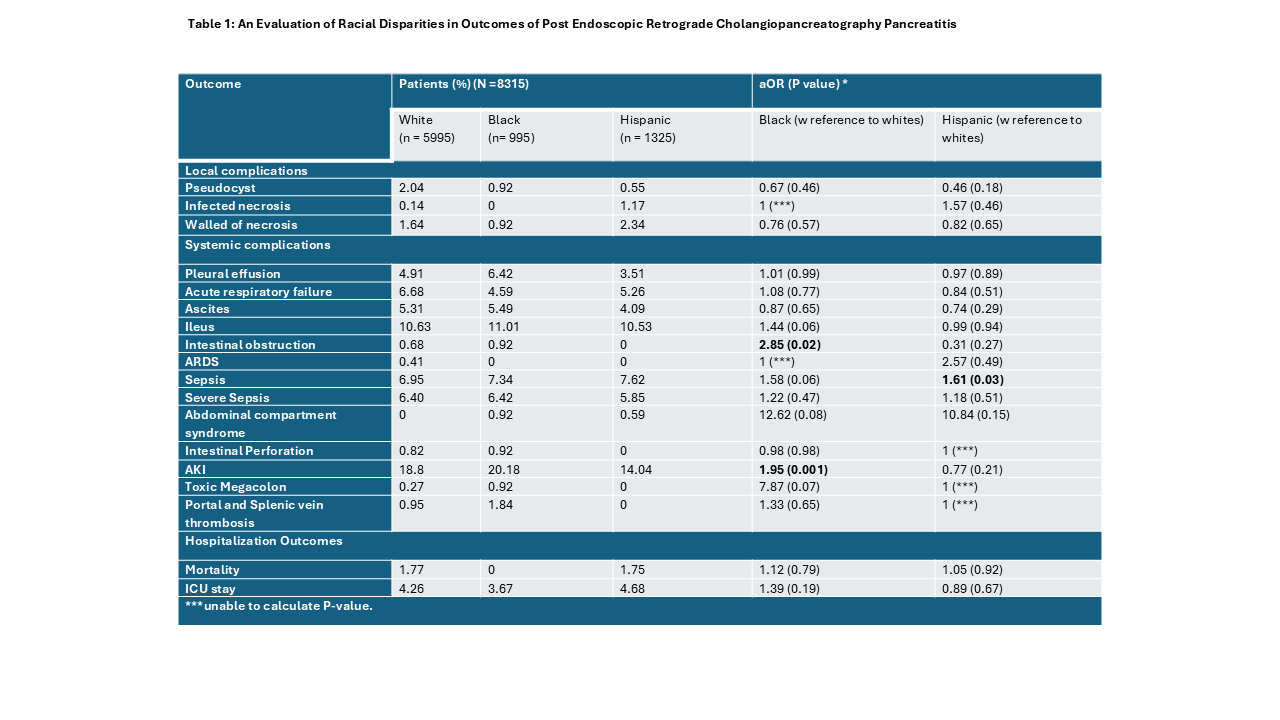
Figure: Table 1
Disclosures:
Amlish Gondal indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Raja Chandra Chakinala indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Ezza Bashir indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Amlish Gondal, MD1, Ali Jaan, MD2, Raja Chandra Chakinala, MD3, Subash Ghimire, MD3, Ezza Bashir, MBBS4, Michael Georgetson, MD, FACG3. P0078 - An Evaluation of Racial Disparities in Outcomes of Post Endoscopic Retrograde Cholangiopancreatography Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
