Sunday Poster Session
Category: Biliary/Pancreas
P0068 - Effectiveness of Invasive Therapies in Chronic Pancreatitis Pain Control: A Systematic Review and Analysis of Clinical Evidence
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Akanksha Togra, MD (she/her/hers)
Texas Tech University Health Sciences Center, El Paso
El Paso, TX
Presenting Author(s)
Akanksha Togra, MD1, Neil Sheth, MD2, Alejandro Robles, MD3, Paul Estrada, MD4, Nirav Thosani, MD5, Sherif E. Elhanafi, MD6
1Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 2McGovern Medical School at UTHealth, Houston, TX; 3Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX; 4Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 5University of Texas Health, McGovern Medical School, Houston, TX; 6Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Management in chronic pancreatitis (CP) focuses on symptomatic relief on pain. High burden and complexity of pain management in CP necessitates a multidisciplinary and mechanism based approach that incorporates procedures in addition to medical, neuromodulatory, or psychological interventions. In this study, we aim to analyze outcomes of invasive therapies such as surgery, endoscopy including Endoscopic Retrograde Cholangiopancreatography (ERCP) / Extracorporeal shockwave lithotripsy (ESWL) and celiac block for CP pain management.
Methods: A systematic PubMed literature search identified 22 randomized controlled trials (RCTs) evaluating pain management strategies in CP. Five of these RCTs were included, pain relief outcomes and responder rates data was extracted. Meta-analyses using random-effects models were conducted to pool results for mean changes in pain scores and responder proportions.
Results: Overall, surgical interventions were superior to endoscopy or celiac plexus block (OR 3.04, 95% CI 1.30–7.07) for managing CP related pain (Figure 1). Among individual procedures, only surgical drainage of the pancreatic duct demonstrated a significant advantage over endoscopic drainage (OR 6.5, 95% CI 1.60–26.36). Although the ESCAPE trial comparing early surgery with an initial endoscopic approach did not show a statistically significant difference (OR 2.11, 95% CI 0.87–5.13), early surgery was associated with lower integrated pain scores over 18 months. Within-group analysis (Figure 2) showed significant improvement in pain scores with pancreaticogastrostomy (MD 84.00, 95% CI 36.18–131.82) and with ESWL plus ERCP (MD 5.20, 95% CI 4.68–5.72). In contrast, celiac plexus block showed no significant benefit (MD 26.00, 95% CI 14.20–66.20). Two additional studies comparing celiac block techniques (Figure 3) also found no significant difference between approaches (OR 1.23, 95% CI 0.42–3.57).
Discussion: This study shows that surgical and endoscopic interventions play a crucial role in the management of CP pain. Celiac block may not be very effective at week 12. Surgical options such as pancreatic duct drainage procedures, and pancreaticogastrostomy are typically useful compared to other methods in cases of the underlying pancreatic morphology and ductal anatomy. Thus, a multidisciplinary strategy that integrates invasive interventions and personalized treatment offers the most effective approach to managing pain in CP.
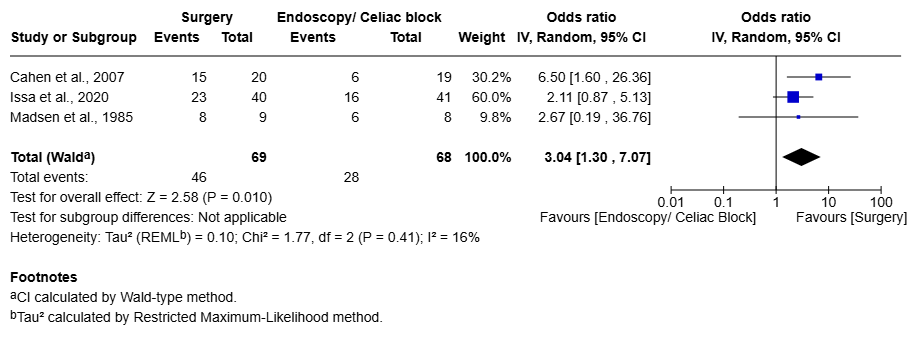
Figure: Figure 1: Comparison of surgical intervention with endoscopy or celiac for pain management
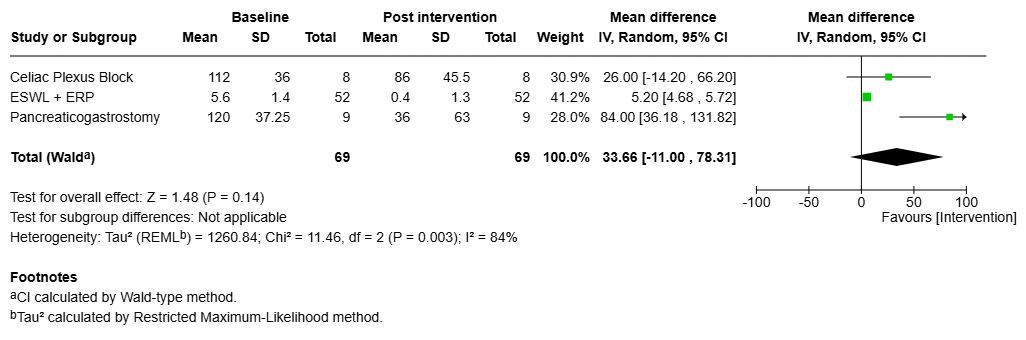
Figure: Figure 2: Within group analysis to assess improvement in pain from baseline
Disclosures:
Akanksha Togra indicated no relevant financial relationships.
Neil Sheth indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Paul Estrada indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Sherif Elhanafi indicated no relevant financial relationships.
Akanksha Togra, MD1, Neil Sheth, MD2, Alejandro Robles, MD3, Paul Estrada, MD4, Nirav Thosani, MD5, Sherif E. Elhanafi, MD6. P0068 - Effectiveness of Invasive Therapies in Chronic Pancreatitis Pain Control: A Systematic Review and Analysis of Clinical Evidence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 2McGovern Medical School at UTHealth, Houston, TX; 3Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX; 4Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 5University of Texas Health, McGovern Medical School, Houston, TX; 6Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Management in chronic pancreatitis (CP) focuses on symptomatic relief on pain. High burden and complexity of pain management in CP necessitates a multidisciplinary and mechanism based approach that incorporates procedures in addition to medical, neuromodulatory, or psychological interventions. In this study, we aim to analyze outcomes of invasive therapies such as surgery, endoscopy including Endoscopic Retrograde Cholangiopancreatography (ERCP) / Extracorporeal shockwave lithotripsy (ESWL) and celiac block for CP pain management.
Methods: A systematic PubMed literature search identified 22 randomized controlled trials (RCTs) evaluating pain management strategies in CP. Five of these RCTs were included, pain relief outcomes and responder rates data was extracted. Meta-analyses using random-effects models were conducted to pool results for mean changes in pain scores and responder proportions.
Results: Overall, surgical interventions were superior to endoscopy or celiac plexus block (OR 3.04, 95% CI 1.30–7.07) for managing CP related pain (Figure 1). Among individual procedures, only surgical drainage of the pancreatic duct demonstrated a significant advantage over endoscopic drainage (OR 6.5, 95% CI 1.60–26.36). Although the ESCAPE trial comparing early surgery with an initial endoscopic approach did not show a statistically significant difference (OR 2.11, 95% CI 0.87–5.13), early surgery was associated with lower integrated pain scores over 18 months. Within-group analysis (Figure 2) showed significant improvement in pain scores with pancreaticogastrostomy (MD 84.00, 95% CI 36.18–131.82) and with ESWL plus ERCP (MD 5.20, 95% CI 4.68–5.72). In contrast, celiac plexus block showed no significant benefit (MD 26.00, 95% CI 14.20–66.20). Two additional studies comparing celiac block techniques (Figure 3) also found no significant difference between approaches (OR 1.23, 95% CI 0.42–3.57).
Discussion: This study shows that surgical and endoscopic interventions play a crucial role in the management of CP pain. Celiac block may not be very effective at week 12. Surgical options such as pancreatic duct drainage procedures, and pancreaticogastrostomy are typically useful compared to other methods in cases of the underlying pancreatic morphology and ductal anatomy. Thus, a multidisciplinary strategy that integrates invasive interventions and personalized treatment offers the most effective approach to managing pain in CP.
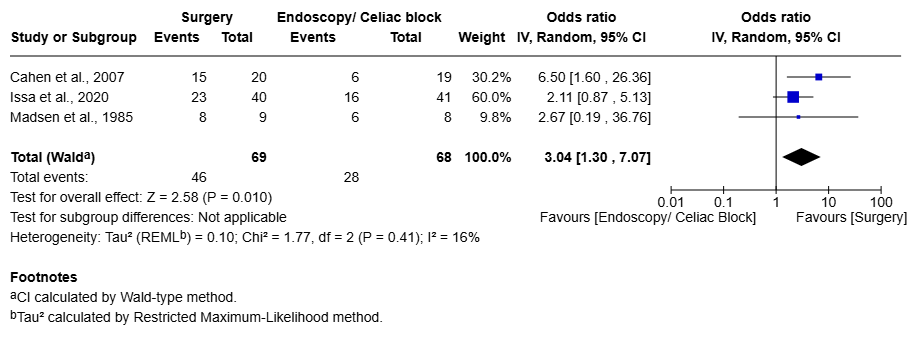
Figure: Figure 1: Comparison of surgical intervention with endoscopy or celiac for pain management
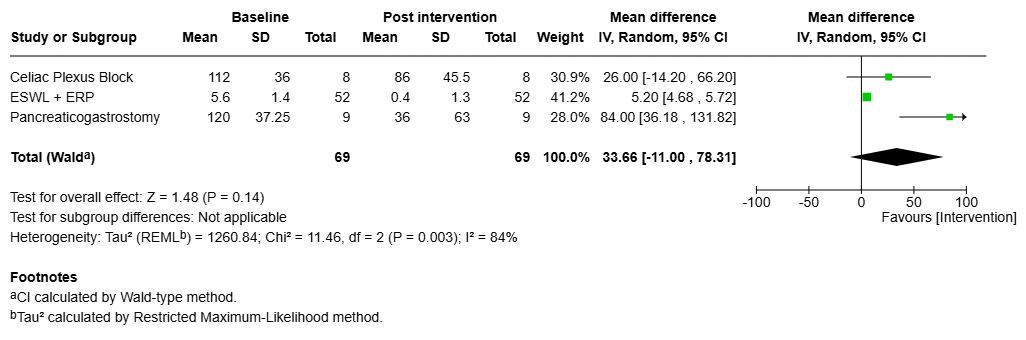
Figure: Figure 2: Within group analysis to assess improvement in pain from baseline
Disclosures:
Akanksha Togra indicated no relevant financial relationships.
Neil Sheth indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Paul Estrada indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Sherif Elhanafi indicated no relevant financial relationships.
Akanksha Togra, MD1, Neil Sheth, MD2, Alejandro Robles, MD3, Paul Estrada, MD4, Nirav Thosani, MD5, Sherif E. Elhanafi, MD6. P0068 - Effectiveness of Invasive Therapies in Chronic Pancreatitis Pain Control: A Systematic Review and Analysis of Clinical Evidence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
