Sunday Poster Session
Category: Biliary/Pancreas
P0063 - Trends in Pancreatitis-Related Mortality in the United States (1999-2024): Disparities by Sex, Race/Ethnicity, Region, and Urbanization
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed B. Elnaggar, MD
Hartford Healthcare
Hartford, CT
Presenting Author(s)
Mohamed A. B. Elnaggar, MD1, Ibrahim Hassan, MBBCh2, Hatem Eltaly, MD3, Mohamed Eldesouki, MD4, Mahmoud Elkammar, MD5, Mohammad Al-Haddad, MD6
1Hartford Healthcare, Hartford, CT; 2Faculty of Medicine, Suez Canal University, Ismailia, Al Isma'iliyah, Egypt; 3Cleveland Clinic Foundation, Cleveland, OH; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5University of Michigan, Ann Arbor, MI; 6Indiana University School of Medicine, Indianapolis, IN
Introduction: Pancreatitis is a serious cause of gastrointestinal morbidity and mortality in the United States. Despite progression in management, trends in pancreatitis-related mortality varies by demographic and geographic factors remain incompletely understood. Our study examined mortality changes for pancreatitis from 1999 to 2024.
Methods: Data extracted on pancreatitis-related deaths from the CDC WONDER database (1999 - 2024) in the U.S. population. Mortality rates were age-adjusted to the 2000 U.S. standard population and expressed per 100,000 persons. Analyses were stratified by
sex (male, female), race/ethnicity (Non-hispanic Black or African American, Non-hispanic White, and Hispanic), region (Northeast, Midwest, South, West), and urbanization (rural vs. urban). Joinpoint regression was employed to identify segments
with distinct trends and estimate Annual Percent Changes (APC). The Average Annual Percent Change (AAPC) was computed to summarize the overall trend during the study period.
Results: The overall AAMR for pancreatitis decreased from 2.61 (95% CI: 2.55–2.67) in 1999 to 1.99 (95% CI: 1.95–2.04) in 2024 (AAPC: –1.14%; 95% CI: –1.36 to –0.91). Analysis showed decline in both females (2.06 to 1.55; AAPC: –1.17%)
and males (3.27 to 2.50; AAPC: –1.09%). Black or African American individuals experienced the most pronounced decrease (4.64 to 2.33; AAPC: –2.81%), followed by Hispanic (2.43 to 1.41; AAPC: –2.58%). White populations showed a
modest reduction (2.36 to 2.14; AAPC: –0.42%).Northeast had the largest overall decline (2.26 to 1.58; AAPC: –1.53%), whereas the Midwest, South, and West showed somewhat smaller negative AAPCs (–0.65%, –1.39%, and –0.71%,
respectively). Urban–rural comparisons indicated a slight increase in rural mortality (2.72 to 2.83; AAPC: 0.03%), contrasted by a decrease in urban areas (2.58 to 2.12; AAPC: –1.03%).
Discussion: Pancreatitis-related mortality in the United States declined overall from 1999 to 2024, with varying degrees of improvement across sex, race/ethnicity, region, and urbanization categories. The relatively high mortality among Black or African American
individuals in 1999 declined sharply than in other groups, while rural areas displayed a stable rates in contrast to the decline in urban areas.These findings highlights targeted public health interventions and resource allocation to address residual disparities, particularly in rural communities and subgroups with persistent or resurgent mortality rates.
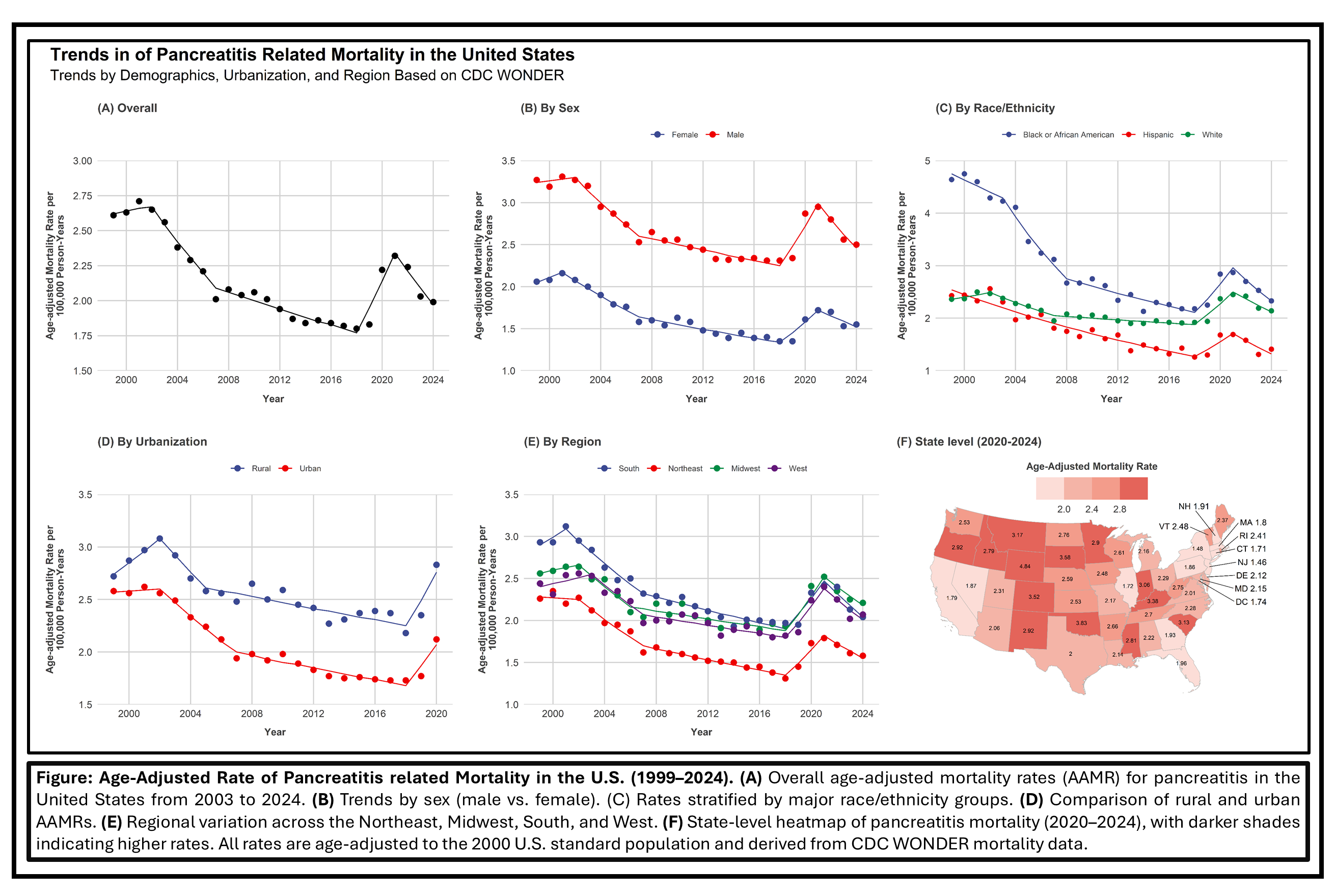
Figure: Trends of Pancreatitis related mortality in the United States
Disclosures:
Mohamed A. Elnaggar indicated no relevant financial relationships.
Ibrahim Hassan indicated no relevant financial relationships.
Hatem Eltaly indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Mahmoud Elkammar indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace diagnostics – Consultant.
Mohamed A. B. Elnaggar, MD1, Ibrahim Hassan, MBBCh2, Hatem Eltaly, MD3, Mohamed Eldesouki, MD4, Mahmoud Elkammar, MD5, Mohammad Al-Haddad, MD6. P0063 - Trends in Pancreatitis-Related Mortality in the United States (1999-2024): Disparities by Sex, Race/Ethnicity, Region, and Urbanization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hartford Healthcare, Hartford, CT; 2Faculty of Medicine, Suez Canal University, Ismailia, Al Isma'iliyah, Egypt; 3Cleveland Clinic Foundation, Cleveland, OH; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5University of Michigan, Ann Arbor, MI; 6Indiana University School of Medicine, Indianapolis, IN
Introduction: Pancreatitis is a serious cause of gastrointestinal morbidity and mortality in the United States. Despite progression in management, trends in pancreatitis-related mortality varies by demographic and geographic factors remain incompletely understood. Our study examined mortality changes for pancreatitis from 1999 to 2024.
Methods: Data extracted on pancreatitis-related deaths from the CDC WONDER database (1999 - 2024) in the U.S. population. Mortality rates were age-adjusted to the 2000 U.S. standard population and expressed per 100,000 persons. Analyses were stratified by
sex (male, female), race/ethnicity (Non-hispanic Black or African American, Non-hispanic White, and Hispanic), region (Northeast, Midwest, South, West), and urbanization (rural vs. urban). Joinpoint regression was employed to identify segments
with distinct trends and estimate Annual Percent Changes (APC). The Average Annual Percent Change (AAPC) was computed to summarize the overall trend during the study period.
Results: The overall AAMR for pancreatitis decreased from 2.61 (95% CI: 2.55–2.67) in 1999 to 1.99 (95% CI: 1.95–2.04) in 2024 (AAPC: –1.14%; 95% CI: –1.36 to –0.91). Analysis showed decline in both females (2.06 to 1.55; AAPC: –1.17%)
and males (3.27 to 2.50; AAPC: –1.09%). Black or African American individuals experienced the most pronounced decrease (4.64 to 2.33; AAPC: –2.81%), followed by Hispanic (2.43 to 1.41; AAPC: –2.58%). White populations showed a
modest reduction (2.36 to 2.14; AAPC: –0.42%).Northeast had the largest overall decline (2.26 to 1.58; AAPC: –1.53%), whereas the Midwest, South, and West showed somewhat smaller negative AAPCs (–0.65%, –1.39%, and –0.71%,
respectively). Urban–rural comparisons indicated a slight increase in rural mortality (2.72 to 2.83; AAPC: 0.03%), contrasted by a decrease in urban areas (2.58 to 2.12; AAPC: –1.03%).
Discussion: Pancreatitis-related mortality in the United States declined overall from 1999 to 2024, with varying degrees of improvement across sex, race/ethnicity, region, and urbanization categories. The relatively high mortality among Black or African American
individuals in 1999 declined sharply than in other groups, while rural areas displayed a stable rates in contrast to the decline in urban areas.These findings highlights targeted public health interventions and resource allocation to address residual disparities, particularly in rural communities and subgroups with persistent or resurgent mortality rates.
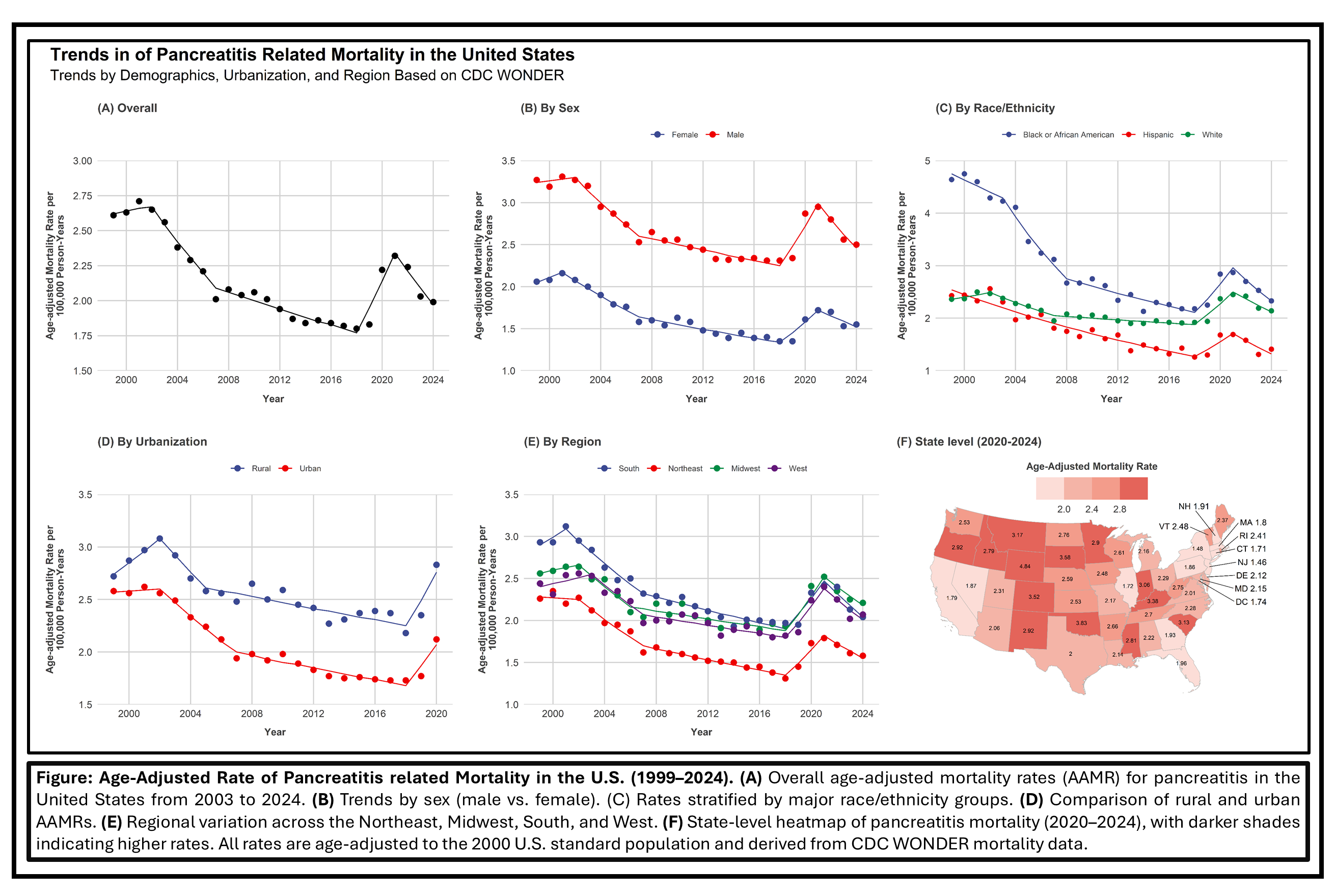
Figure: Trends of Pancreatitis related mortality in the United States
Disclosures:
Mohamed A. Elnaggar indicated no relevant financial relationships.
Ibrahim Hassan indicated no relevant financial relationships.
Hatem Eltaly indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Mahmoud Elkammar indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace diagnostics – Consultant.
Mohamed A. B. Elnaggar, MD1, Ibrahim Hassan, MBBCh2, Hatem Eltaly, MD3, Mohamed Eldesouki, MD4, Mahmoud Elkammar, MD5, Mohammad Al-Haddad, MD6. P0063 - Trends in Pancreatitis-Related Mortality in the United States (1999-2024): Disparities by Sex, Race/Ethnicity, Region, and Urbanization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
