Sunday Poster Session
Category: Biliary/Pancreas
P0036 - Does Obesity Affect ERCP Outcomes in Acute Cholangitis? A Propensity Matched Study Using National Readmission Database 2018-2020
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Madhav Changela, MD
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Madhav Changela, MD1, Janak Bahirwani, MD2, Nishit Patel, MD3, Maulik Kaneriya, MD1, Krishna Bodrya, MD4, Yasir Ali, MD5, Yecheskel Schneider, MD, MS6
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Kadlec Regional Medical Center, Richland, WA; 3St. Luke's University Health Network, Bethlehem, PA; 4Leigh Valley Health Network, Easton, PA; 5One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 6Virtua Health System, Moorestown, NJ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a widely utilized diagnostic and therapeutic intervention for management of acute cholangitis. With increasing prevalence of obesity, a considerable number of acute cholangitis patients also present with a secondary diagnosis of obesity. This retrospective study aims to assess the impact of obesity on the periprocedural outcomes of ERCP in acute cholangitis.
Methods: This is a retrospective analysis using data from the National Readmission Database (NRD) for the years 2018-2020. It included all patients aged over 18 years who were admitted for acute cholangitis and underwent ERCP. These patients were stratified into two groups based on the presence of obesity. Primary outcomes were mortality and the all-cause 30-day readmission rate. Secondary outcomes included length of stay (LOS), total hospitalization charges, sepsis, post ERCP hemorrhage, post ERCP pancreatitis. Multivariate regression model was used to evaluate the outcomes among two cohorts after adjusting for potential confounders. To further address the bias, propensity scores were estimated by incorporating relevant baseline covariates. Matched cohort were then used to compare outcomes. P value < 0.05 was considered statistically significant.
Results: A total of 23052 acute cholangitis patients underwent ECRP among whom 4129(17.91%) patients were obese. Basic demographic characteristics are summarized in Table 1, while detailed clinical outcomes are presented in Table 2. Compared to non-obese, obese patient cohort was associated with a lower odd of mortality, and higher odds of sepsis. Obese patient cohort was associated with higher total hospitalization charges and longer length of stay compared to non-obese one. Most common causes of readmission were recurrence of cholangitis and sepsis, acute pancreatitis, and bile duct obstruction. Statistically significant independent predictors of 30-day all-cause readmissions following ERCP in acute cholangitis included obesity, advanced age, a high Charlson comorbidity index, malignant bile duct neoplasm, and John Hopkins ACG frailty.
Discussion: Our study shows higher odds of sepsis and total hospitalization charges and lower odds of in-hospital mortality and 30-day all cause readmission rate among obese patients undergoing ERCP in acute cholangitis compared to non-obese cohort. While this study provides valuable insights into the management of acute cholangitis with obesity, further research is required to support the findings.
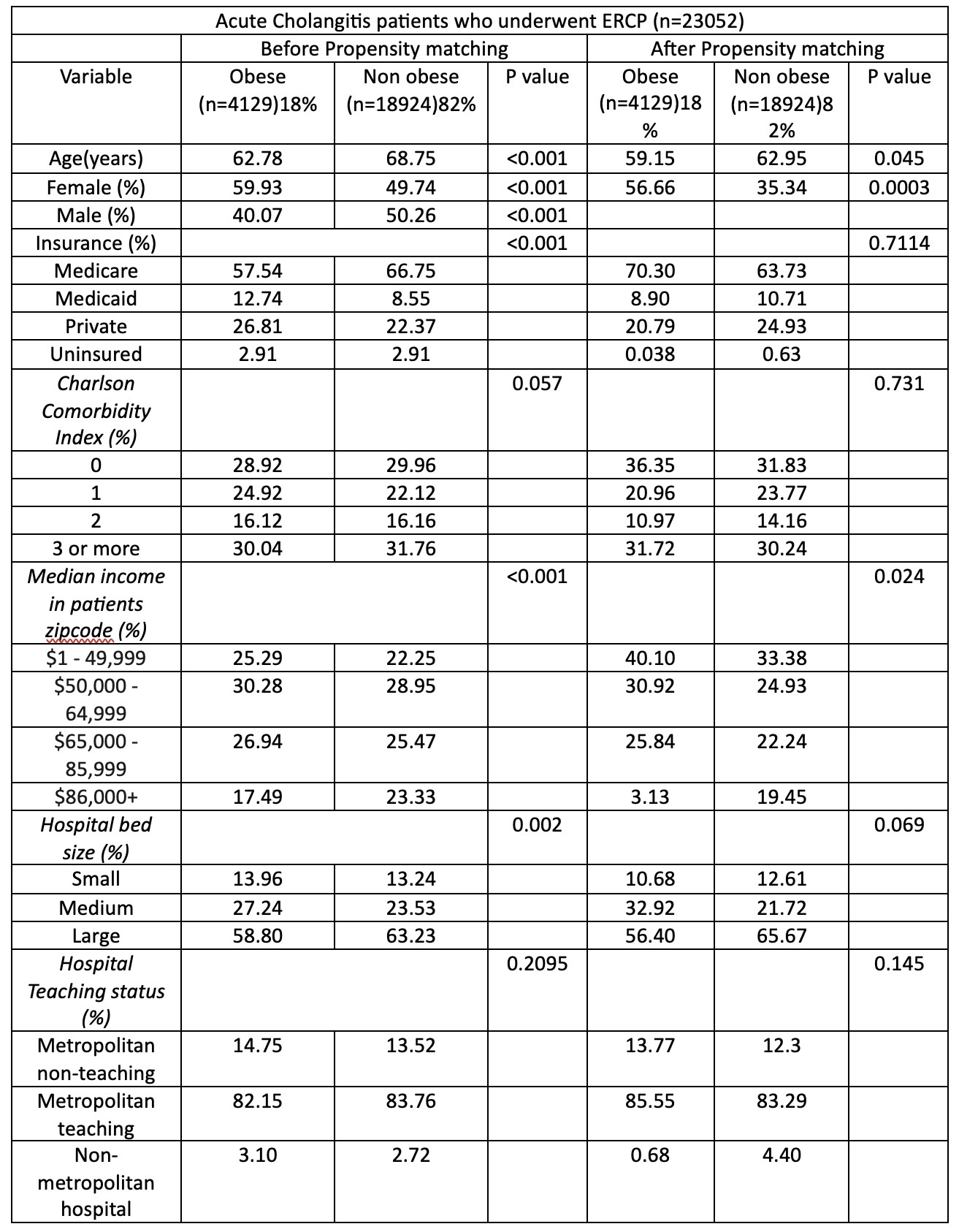
Figure: Table 1: Patient demographic characteristics.
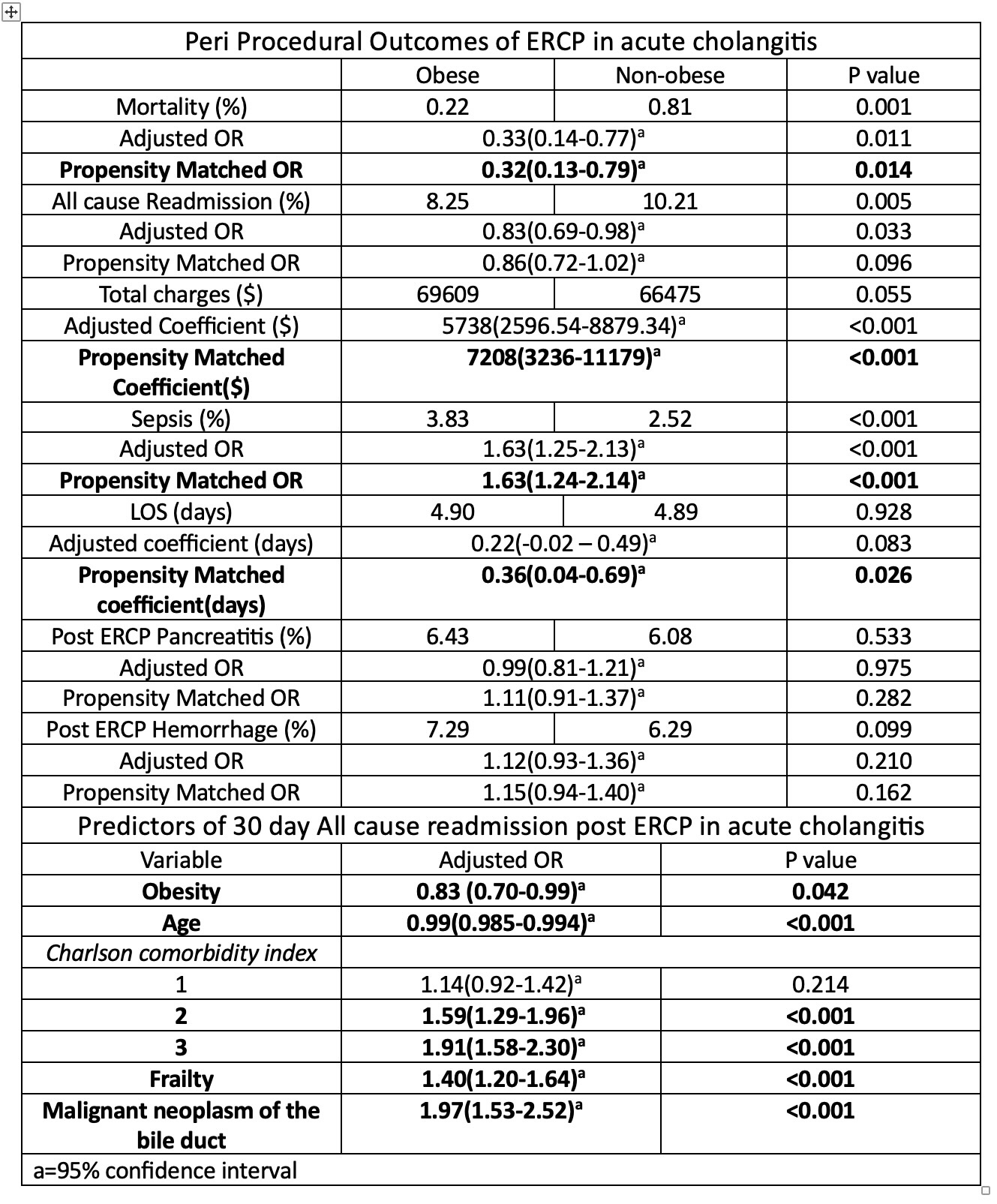
Figure: Table 2: Clinical Outcomes and Predictors of 30 day all cause readmissions post ERCP in acute cholangitis.
Disclosures:
Madhav Changela indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Maulik Kaneriya indicated no relevant financial relationships.
Krishna Bodrya indicated no relevant financial relationships.
Yasir Ali indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Madhav Changela, MD1, Janak Bahirwani, MD2, Nishit Patel, MD3, Maulik Kaneriya, MD1, Krishna Bodrya, MD4, Yasir Ali, MD5, Yecheskel Schneider, MD, MS6. P0036 - Does Obesity Affect ERCP Outcomes in Acute Cholangitis? A Propensity Matched Study Using National Readmission Database 2018-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Kadlec Regional Medical Center, Richland, WA; 3St. Luke's University Health Network, Bethlehem, PA; 4Leigh Valley Health Network, Easton, PA; 5One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 6Virtua Health System, Moorestown, NJ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a widely utilized diagnostic and therapeutic intervention for management of acute cholangitis. With increasing prevalence of obesity, a considerable number of acute cholangitis patients also present with a secondary diagnosis of obesity. This retrospective study aims to assess the impact of obesity on the periprocedural outcomes of ERCP in acute cholangitis.
Methods: This is a retrospective analysis using data from the National Readmission Database (NRD) for the years 2018-2020. It included all patients aged over 18 years who were admitted for acute cholangitis and underwent ERCP. These patients were stratified into two groups based on the presence of obesity. Primary outcomes were mortality and the all-cause 30-day readmission rate. Secondary outcomes included length of stay (LOS), total hospitalization charges, sepsis, post ERCP hemorrhage, post ERCP pancreatitis. Multivariate regression model was used to evaluate the outcomes among two cohorts after adjusting for potential confounders. To further address the bias, propensity scores were estimated by incorporating relevant baseline covariates. Matched cohort were then used to compare outcomes. P value < 0.05 was considered statistically significant.
Results: A total of 23052 acute cholangitis patients underwent ECRP among whom 4129(17.91%) patients were obese. Basic demographic characteristics are summarized in Table 1, while detailed clinical outcomes are presented in Table 2. Compared to non-obese, obese patient cohort was associated with a lower odd of mortality, and higher odds of sepsis. Obese patient cohort was associated with higher total hospitalization charges and longer length of stay compared to non-obese one. Most common causes of readmission were recurrence of cholangitis and sepsis, acute pancreatitis, and bile duct obstruction. Statistically significant independent predictors of 30-day all-cause readmissions following ERCP in acute cholangitis included obesity, advanced age, a high Charlson comorbidity index, malignant bile duct neoplasm, and John Hopkins ACG frailty.
Discussion: Our study shows higher odds of sepsis and total hospitalization charges and lower odds of in-hospital mortality and 30-day all cause readmission rate among obese patients undergoing ERCP in acute cholangitis compared to non-obese cohort. While this study provides valuable insights into the management of acute cholangitis with obesity, further research is required to support the findings.
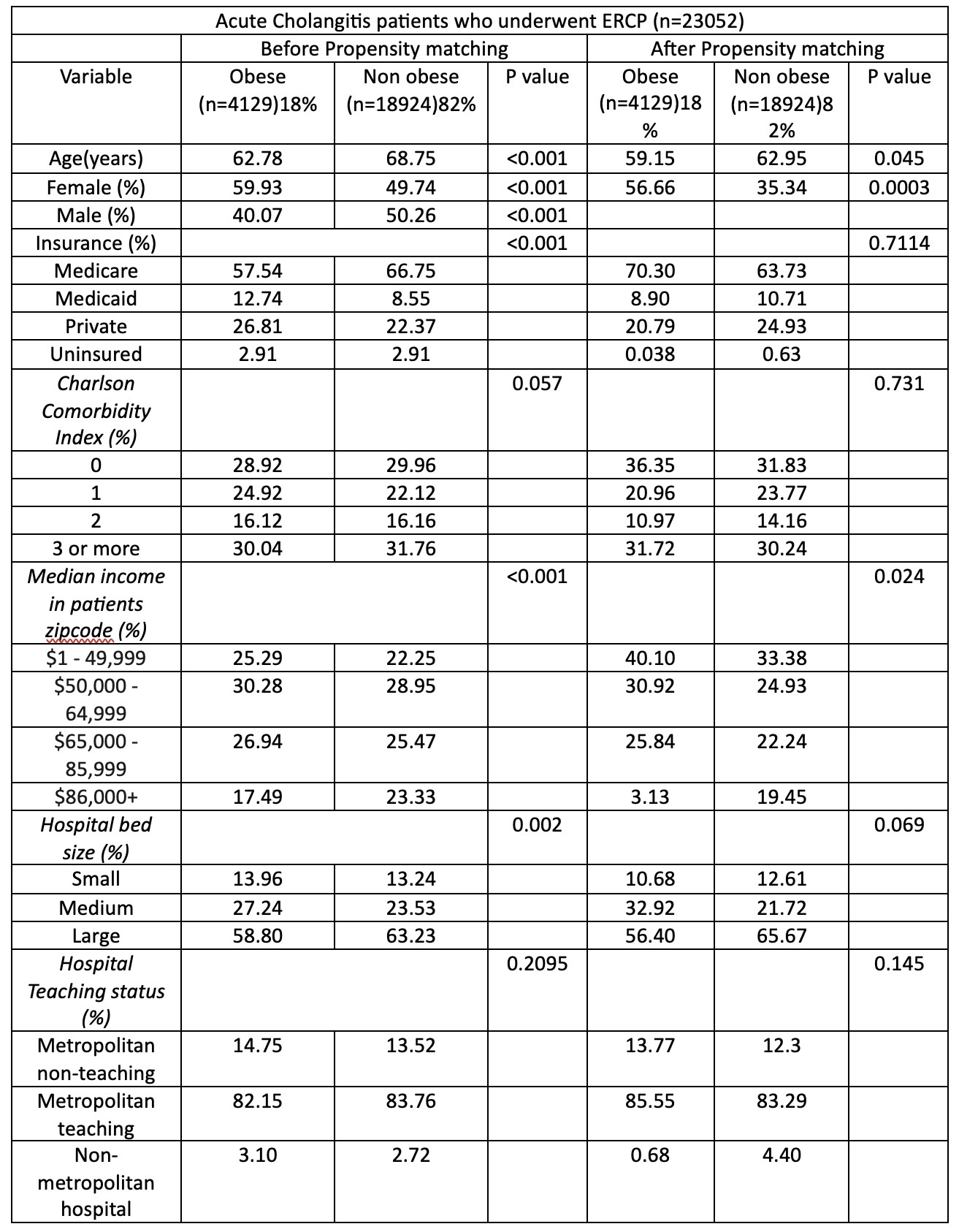
Figure: Table 1: Patient demographic characteristics.
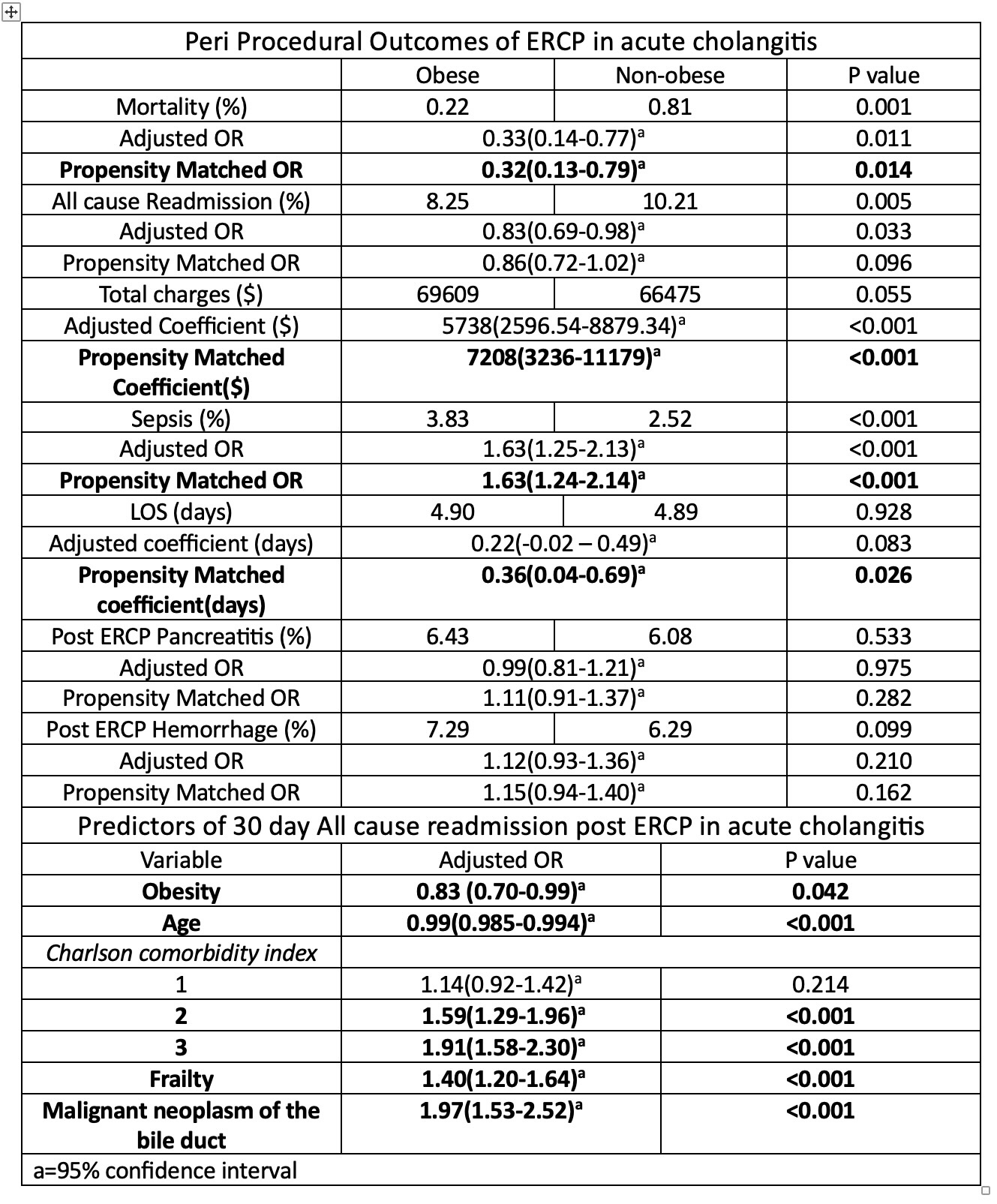
Figure: Table 2: Clinical Outcomes and Predictors of 30 day all cause readmissions post ERCP in acute cholangitis.
Disclosures:
Madhav Changela indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Maulik Kaneriya indicated no relevant financial relationships.
Krishna Bodrya indicated no relevant financial relationships.
Yasir Ali indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Madhav Changela, MD1, Janak Bahirwani, MD2, Nishit Patel, MD3, Maulik Kaneriya, MD1, Krishna Bodrya, MD4, Yasir Ali, MD5, Yecheskel Schneider, MD, MS6. P0036 - Does Obesity Affect ERCP Outcomes in Acute Cholangitis? A Propensity Matched Study Using National Readmission Database 2018-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
