Sunday Poster Session
Category: Biliary/Pancreas
P0035 - Determinants of Overall Survival in Veterans with Pancreatic Cancer: The Impact of Demographics, Comorbidities, and Treatment Modalities
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Akhil Adla, DO
University of Tennessee Health Science Center
Memphis, TN
Presenting Author(s)
Akhil Adla, DO1, Hayes Walker, MD2, Louis Yn, MD3, Samantha Whitwell, MD2, Claudio Tombazzi, MD4
1University of Tennessee Health Science Center, Memphis, TN; 2UTHSC, Memphis, TN; 3University of Tennessee Health Science Center - Methodist University Hospital, Memphis, TN; 4VA Memphis Health Care, Memphis, TN
Introduction: Pancreatic cancer remains a leading cause of cancer mortality [3]. In veterans, variables such as rural or urban, race, residence may reflect access to care and survival outcomes. Tobacco, alcohol use, obesity, comorbidities, family history, race and sex are the major risk factors for developing pancreatic cancer [1][2]. Receipt of chemotherapy, surgery, or radiation is associated with improved survival. Understanding these determinants is essential for addressing disparities and improving outcomes in this high-risk population.
Methods: A retrospective chart review was conducted of veterans diagnosed with pancreatic cancer from 2014 to 2024, utilizing the Computerized Patient Record System (CPRS) within the Veterans Health Administration (VHA). Observed variables included age, sex, race/ethnicity, stage at diagnosis, comorbidities and modifiable risk factors, treatment modalities, and survival. Comparative analyses were performed to assess associations among these factors.
Results: Overall, from 2014 to 2024, 118 patients were diagnosed with pancreatic cancer, with a significant male predominance (98.1%). Mean overall survival (OS) of patients was 16.8 months and median OS of 7.5 months with a 95% confidence interval of 390 – 630.3 days. A total of 96% of patients underwent chemotherapy, 8.5% underwent surgery, and 9.4% received radiation. The mean surgical patient OS of 47.1 months far exceeded the mean OS of non-surgical patients at 9.2 months (p=< 0.0001). Patients who received longer duration of chemotherapy had longer overall survival. Urban patients had a mean OS of 481 days versus 572 days for rural patients (p= >0.05). Patients who admitted to alcohol use had a mean overall survival rate of 10.5 compared to 22.7 for non-alcohol users. No statistically significant difference in overall survival was observed between tobacco users versus non-tobacco users.
Discussion: Patient survival remains similar to the data seen at the larger population level, suggesting veterans receive the standard of care. In contrast to existing data, there has been no statistically significant overall survival difference observed between tobacco and non-tobacco users. Only 8.5% of patients received surgery, underscoring that initial diagnosis for most patients in this cohort occurred at advanced stages of the disease. The difference in overall survival between surgical and non-surgical patients highlights the need for sensitive screening methods to diagnose this disease earlier in its course.
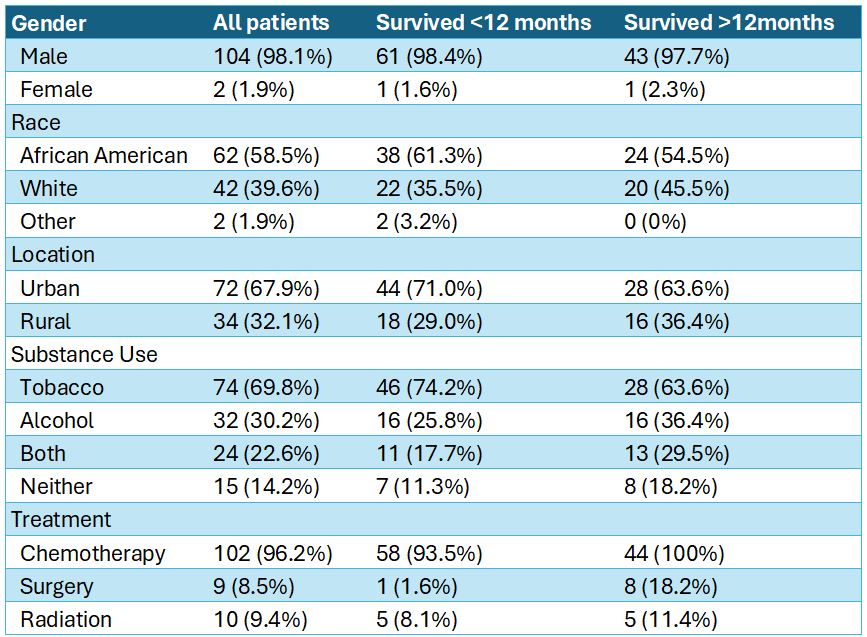
Figure: Figure A: Majority of pancreatic patients in the study were men and only 8.5% total patients received surgery.
Disclosures:
Akhil Adla indicated no relevant financial relationships.
Hayes Walker indicated no relevant financial relationships.
Louis Yn indicated no relevant financial relationships.
Samantha Whitwell indicated no relevant financial relationships.
Claudio Tombazzi indicated no relevant financial relationships.
Akhil Adla, DO1, Hayes Walker, MD2, Louis Yn, MD3, Samantha Whitwell, MD2, Claudio Tombazzi, MD4. P0035 - Determinants of Overall Survival in Veterans with Pancreatic Cancer: The Impact of Demographics, Comorbidities, and Treatment Modalities, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Tennessee Health Science Center, Memphis, TN; 2UTHSC, Memphis, TN; 3University of Tennessee Health Science Center - Methodist University Hospital, Memphis, TN; 4VA Memphis Health Care, Memphis, TN
Introduction: Pancreatic cancer remains a leading cause of cancer mortality [3]. In veterans, variables such as rural or urban, race, residence may reflect access to care and survival outcomes. Tobacco, alcohol use, obesity, comorbidities, family history, race and sex are the major risk factors for developing pancreatic cancer [1][2]. Receipt of chemotherapy, surgery, or radiation is associated with improved survival. Understanding these determinants is essential for addressing disparities and improving outcomes in this high-risk population.
Methods: A retrospective chart review was conducted of veterans diagnosed with pancreatic cancer from 2014 to 2024, utilizing the Computerized Patient Record System (CPRS) within the Veterans Health Administration (VHA). Observed variables included age, sex, race/ethnicity, stage at diagnosis, comorbidities and modifiable risk factors, treatment modalities, and survival. Comparative analyses were performed to assess associations among these factors.
Results: Overall, from 2014 to 2024, 118 patients were diagnosed with pancreatic cancer, with a significant male predominance (98.1%). Mean overall survival (OS) of patients was 16.8 months and median OS of 7.5 months with a 95% confidence interval of 390 – 630.3 days. A total of 96% of patients underwent chemotherapy, 8.5% underwent surgery, and 9.4% received radiation. The mean surgical patient OS of 47.1 months far exceeded the mean OS of non-surgical patients at 9.2 months (p=< 0.0001). Patients who received longer duration of chemotherapy had longer overall survival. Urban patients had a mean OS of 481 days versus 572 days for rural patients (p= >0.05). Patients who admitted to alcohol use had a mean overall survival rate of 10.5 compared to 22.7 for non-alcohol users. No statistically significant difference in overall survival was observed between tobacco users versus non-tobacco users.
Discussion: Patient survival remains similar to the data seen at the larger population level, suggesting veterans receive the standard of care. In contrast to existing data, there has been no statistically significant overall survival difference observed between tobacco and non-tobacco users. Only 8.5% of patients received surgery, underscoring that initial diagnosis for most patients in this cohort occurred at advanced stages of the disease. The difference in overall survival between surgical and non-surgical patients highlights the need for sensitive screening methods to diagnose this disease earlier in its course.
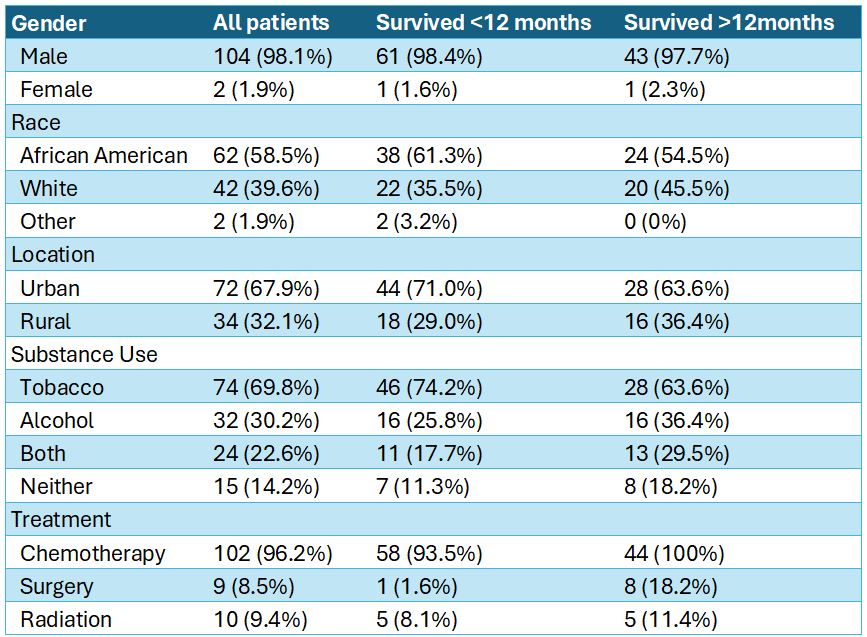
Figure: Figure A: Majority of pancreatic patients in the study were men and only 8.5% total patients received surgery.
Disclosures:
Akhil Adla indicated no relevant financial relationships.
Hayes Walker indicated no relevant financial relationships.
Louis Yn indicated no relevant financial relationships.
Samantha Whitwell indicated no relevant financial relationships.
Claudio Tombazzi indicated no relevant financial relationships.
Akhil Adla, DO1, Hayes Walker, MD2, Louis Yn, MD3, Samantha Whitwell, MD2, Claudio Tombazzi, MD4. P0035 - Determinants of Overall Survival in Veterans with Pancreatic Cancer: The Impact of Demographics, Comorbidities, and Treatment Modalities, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
