Sunday Poster Session
Category: Biliary/Pancreas
P0031 - Evolving Risk Profiles in Pancreatic Cancer: US Trends in Mortality Attributable to Smoking and Hyperglycemia (2000-2021)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Urmimala Chaudhuri, DO
Wright State University
Centerville, OH
Presenting Author(s)
Urmimala Chaudhuri, DO1, Drew Triplett, DO2
1Wright State University, Centerville, OH; 2Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Pancreatic cancer remains one of the most lethal gastrointestinal malignancies, with a five-year
survival rate below 10%. As gastroenterologists increasingly participate in the surveillance and
risk assessment of patients at elevated risk of pancreatic cancer, particularly through diagnostic
procedures and management of comorbid GI conditions, understanding evolving contributors to
mortality is essential. This study examines trends in pancreatic cancer mortality attributable to
two significant risk factors: smoking and high fasting plasma glucose (HFPG) in the United
States from 2000 to 2021.
Methods: We analyzed age-adjusted pancreatic mortality rates attributable to smoking and high fasting
plasma glucose from 2000 to 2021 utilizing the Global Burden of Disease (GBD) database.
Temporal trends were evaluated using Joinpoint regression to calculate annual percent changes
(APC) and average annual percentage changes (AAPC), with statistical significance set at
p< 0.05.
Results: Pancreatic cancer mortality attributable to smoking showed a modest but statistically significant
increase from 2003 to 2016 (APC: 0.45%, p< 0.05), followed by a plateau from 2016 to 2021. In
contrast, mortality attributable to HFPG rose sharply between 2000 and 2005 (APC: 3.83%,
p< 0.05) and continued to increase through 2021, albeit more gradually (APC: 2.06%, p< 0.05).
Over the entire period, the AAPC for HFPG (2.86%, p< 0.05) significantly exceeded that of
smoking (0.71%, p< 0.05), indicating a shift in dominant risk factors.
Discussion: Our study highlights the shifting landscape of pancreatic cancer mortality risk factors. While
smoking-related deaths have stabilized-likely reflecting effective public health policies-the
contribution of hyperglycemia has risen consistently. The sustained rise in mortality linked to
hyperglycemia reveals a growing and underrecognized burden. Interestingly, HFPG emerged as
a dominant contributor with a consistently higher AAPC across the study period. This trend
emphasizes the urgent need to integrate metabolic health strategies into GI cancer prevention
frameworks. Gastroenterologists are uniquely positioned to integrate metabolic and lifestyle
counseling in the care of patients at risk for GI malignancies.
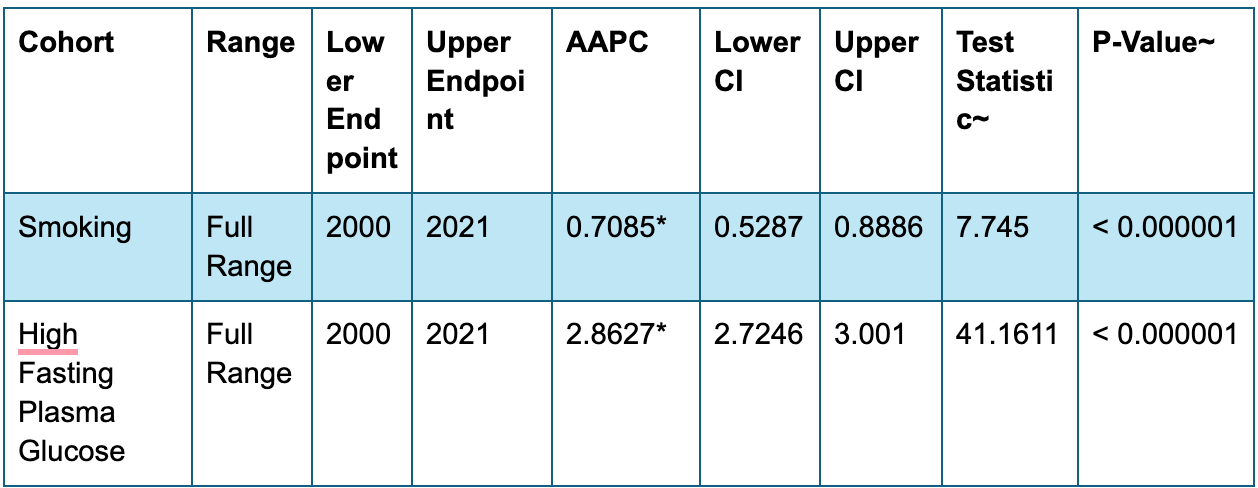
Figure: Joinpoint regression showing the increasing pancreatic cancer burden from 2000–2021 attributable to smoking and high fasting plasma glucose.
Disclosures:
Urmimala Chaudhuri indicated no relevant financial relationships.
Drew Triplett indicated no relevant financial relationships.
Urmimala Chaudhuri, DO1, Drew Triplett, DO2. P0031 - Evolving Risk Profiles in Pancreatic Cancer: US Trends in Mortality Attributable to Smoking and Hyperglycemia (2000-2021), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright State University, Centerville, OH; 2Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Pancreatic cancer remains one of the most lethal gastrointestinal malignancies, with a five-year
survival rate below 10%. As gastroenterologists increasingly participate in the surveillance and
risk assessment of patients at elevated risk of pancreatic cancer, particularly through diagnostic
procedures and management of comorbid GI conditions, understanding evolving contributors to
mortality is essential. This study examines trends in pancreatic cancer mortality attributable to
two significant risk factors: smoking and high fasting plasma glucose (HFPG) in the United
States from 2000 to 2021.
Methods: We analyzed age-adjusted pancreatic mortality rates attributable to smoking and high fasting
plasma glucose from 2000 to 2021 utilizing the Global Burden of Disease (GBD) database.
Temporal trends were evaluated using Joinpoint regression to calculate annual percent changes
(APC) and average annual percentage changes (AAPC), with statistical significance set at
p< 0.05.
Results: Pancreatic cancer mortality attributable to smoking showed a modest but statistically significant
increase from 2003 to 2016 (APC: 0.45%, p< 0.05), followed by a plateau from 2016 to 2021. In
contrast, mortality attributable to HFPG rose sharply between 2000 and 2005 (APC: 3.83%,
p< 0.05) and continued to increase through 2021, albeit more gradually (APC: 2.06%, p< 0.05).
Over the entire period, the AAPC for HFPG (2.86%, p< 0.05) significantly exceeded that of
smoking (0.71%, p< 0.05), indicating a shift in dominant risk factors.
Discussion: Our study highlights the shifting landscape of pancreatic cancer mortality risk factors. While
smoking-related deaths have stabilized-likely reflecting effective public health policies-the
contribution of hyperglycemia has risen consistently. The sustained rise in mortality linked to
hyperglycemia reveals a growing and underrecognized burden. Interestingly, HFPG emerged as
a dominant contributor with a consistently higher AAPC across the study period. This trend
emphasizes the urgent need to integrate metabolic health strategies into GI cancer prevention
frameworks. Gastroenterologists are uniquely positioned to integrate metabolic and lifestyle
counseling in the care of patients at risk for GI malignancies.
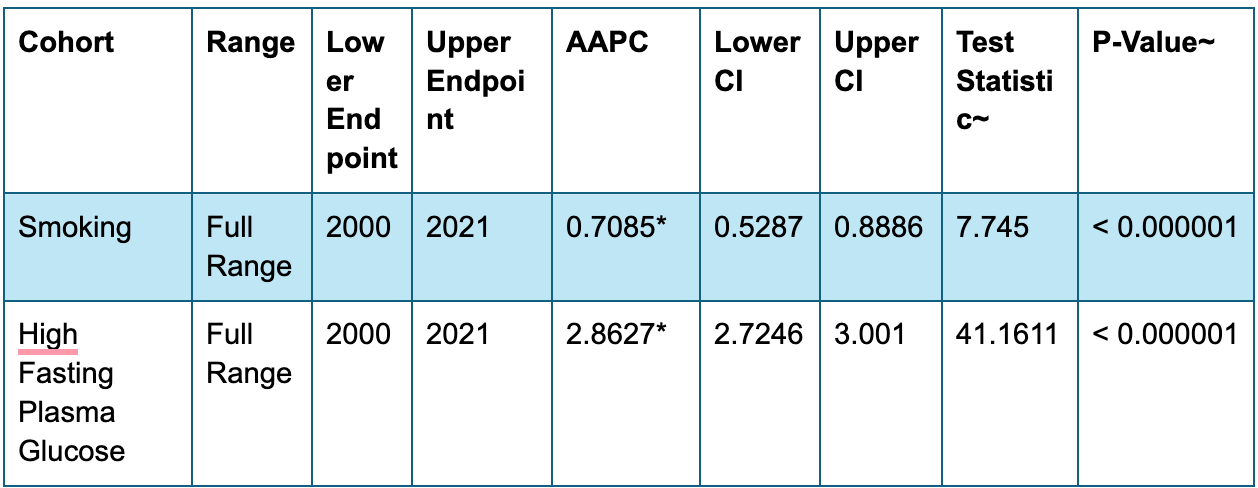
Figure: Joinpoint regression showing the increasing pancreatic cancer burden from 2000–2021 attributable to smoking and high fasting plasma glucose.
Disclosures:
Urmimala Chaudhuri indicated no relevant financial relationships.
Drew Triplett indicated no relevant financial relationships.
Urmimala Chaudhuri, DO1, Drew Triplett, DO2. P0031 - Evolving Risk Profiles in Pancreatic Cancer: US Trends in Mortality Attributable to Smoking and Hyperglycemia (2000-2021), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
