Sunday Poster Session
Category: Biliary/Pancreas
P0024 - Mapping Hidden Type 3c Diabetes Across the United States
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JA
John K. Appiah, MD
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
John K. Appiah, MD1, Ewurabena N. Plange-Kaye, DDS2, Chukwunonso Ubanatu, MD1, George S. Blewusi, MD3, Emmanuel Asare, 4
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Columbia University, Dumont, NJ; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 4Montefiore hospital, Bronx, NY
Introduction: Type 3c diabetes (pancreatic diabetes) may comprise 8% of all diabetes cases but remains underdiagnosed. This study develops a novel diagnostic gap methodology integrating pancreatic cancer mortality, diabetes mortality, and pancreatitis prevalence to identify geographic areas with systematic Type 3c diabetes underrecognition.
Methods: We conducted a comprehensive analysis integrating CDC WONDER mortality data (2018-2023) for pancreatic cancer (ICD-10: C25) and diabetes mellitus (ICD-10: E10-E14) with Global Burden of Disease (GBD) 2019 prevalence estimates for pancreatitis and diabetes across 51 US states/territories. A novel diagnostic gap score was calculated as: (pancreatic cancer/diabetes mortality ratio) - (pancreatitis/diabetes prevalence ratio) to identify states with disproportionate pancreatic cancer mortality after controlling for underlying pancreatic disease burden.
Results: Analysis included 283,255 pancreatic cancer deaths, 574,474 diabetes deaths (CDC WONDER), and state-level prevalence data for 6.6 million pancreatitis cases and 166 million diabetes cases (GBD 2019). Diagnostic gap scores varied significantly from 28.1% to 71.4% (mean: 48.2%, SD: 9.4%, CV: 19.5%). Five states showed statistically significant underdiagnosis (gap score >62.3%): Connecticut (71.4%), Massachusetts (70.3%), Vermont (66.1%), New Jersey (63.8%), and Hawaii (63.5%). Three states demonstrated superior recognition (gap score < 34.1%): West Virginia (28.1%), Arkansas (32.0%), and New Mexico (33.6%). The diagnostic gap score methodology controls for underlying pancreatic disease burden, providing more precise identification of diagnostic disparities than mortality ratios alone.
Discussion: A novel diagnostic gap score reveals significant geographic disparities in Type 3c diabetes recognition. Five states (Connecticut, Massachusetts, Vermont, New Jersey, Hawaii) show marked underdiagnosis, while three (West Virginia, Arkansas, New Mexico) demonstrate better diagnostic alignment. These findings highlight Northeast states as priority targets for intervention and offer a framework for tracking diagnostic quality. Future studies should validate this methodology using electronic health record data and investigate targeted provider education interventions in high-gap states.
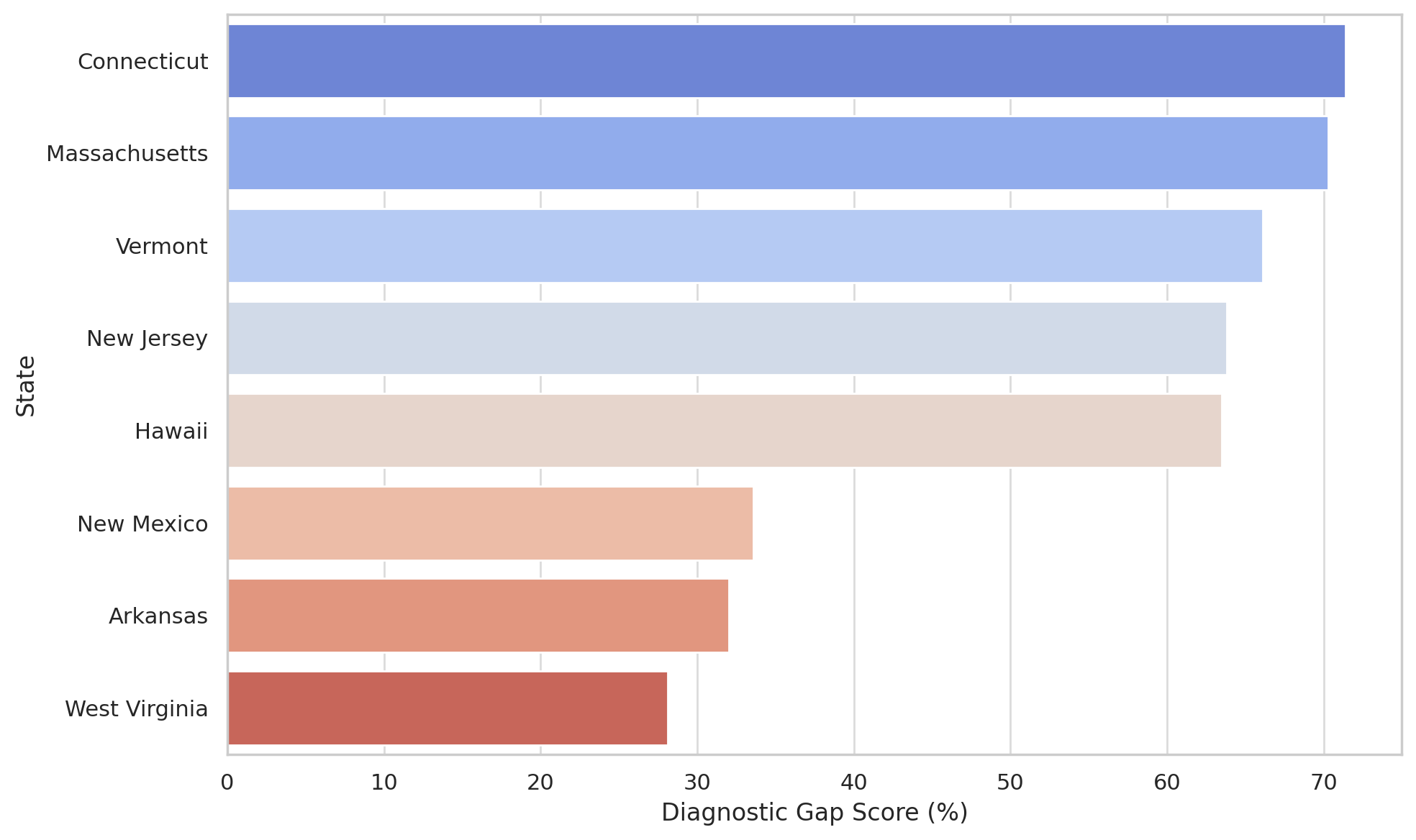
Figure: Figure 1: Adjusted Diagnostic Gap Scores for Selected U.S. States.
States with the highest scores (Connecticut, Massachusetts, Vermont, New Jersey, and Hawaii) demonstrate disproportionately high pancreatic cancer mortality relative to diabetes mortality and pancreatitis prevalence, indicating potential underdiagnosis of type 3c diabetes. In contrast, West Virginia, Arkansas, and New Mexico show lower gap scores, suggesting better recognition and diagnostic alignment. Scores are rounded to match values reported in the abstract.
Disclosures:
John Appiah indicated no relevant financial relationships.
Ewurabena Plange-Kaye indicated no relevant financial relationships.
Chukwunonso Ubanatu indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Emmanuel Asare indicated no relevant financial relationships.
John K. Appiah, MD1, Ewurabena N. Plange-Kaye, DDS2, Chukwunonso Ubanatu, MD1, George S. Blewusi, MD3, Emmanuel Asare, 4. P0024 - Mapping Hidden Type 3c Diabetes Across the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Columbia University, Dumont, NJ; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 4Montefiore hospital, Bronx, NY
Introduction: Type 3c diabetes (pancreatic diabetes) may comprise 8% of all diabetes cases but remains underdiagnosed. This study develops a novel diagnostic gap methodology integrating pancreatic cancer mortality, diabetes mortality, and pancreatitis prevalence to identify geographic areas with systematic Type 3c diabetes underrecognition.
Methods: We conducted a comprehensive analysis integrating CDC WONDER mortality data (2018-2023) for pancreatic cancer (ICD-10: C25) and diabetes mellitus (ICD-10: E10-E14) with Global Burden of Disease (GBD) 2019 prevalence estimates for pancreatitis and diabetes across 51 US states/territories. A novel diagnostic gap score was calculated as: (pancreatic cancer/diabetes mortality ratio) - (pancreatitis/diabetes prevalence ratio) to identify states with disproportionate pancreatic cancer mortality after controlling for underlying pancreatic disease burden.
Results: Analysis included 283,255 pancreatic cancer deaths, 574,474 diabetes deaths (CDC WONDER), and state-level prevalence data for 6.6 million pancreatitis cases and 166 million diabetes cases (GBD 2019). Diagnostic gap scores varied significantly from 28.1% to 71.4% (mean: 48.2%, SD: 9.4%, CV: 19.5%). Five states showed statistically significant underdiagnosis (gap score >62.3%): Connecticut (71.4%), Massachusetts (70.3%), Vermont (66.1%), New Jersey (63.8%), and Hawaii (63.5%). Three states demonstrated superior recognition (gap score < 34.1%): West Virginia (28.1%), Arkansas (32.0%), and New Mexico (33.6%). The diagnostic gap score methodology controls for underlying pancreatic disease burden, providing more precise identification of diagnostic disparities than mortality ratios alone.
Discussion: A novel diagnostic gap score reveals significant geographic disparities in Type 3c diabetes recognition. Five states (Connecticut, Massachusetts, Vermont, New Jersey, Hawaii) show marked underdiagnosis, while three (West Virginia, Arkansas, New Mexico) demonstrate better diagnostic alignment. These findings highlight Northeast states as priority targets for intervention and offer a framework for tracking diagnostic quality. Future studies should validate this methodology using electronic health record data and investigate targeted provider education interventions in high-gap states.
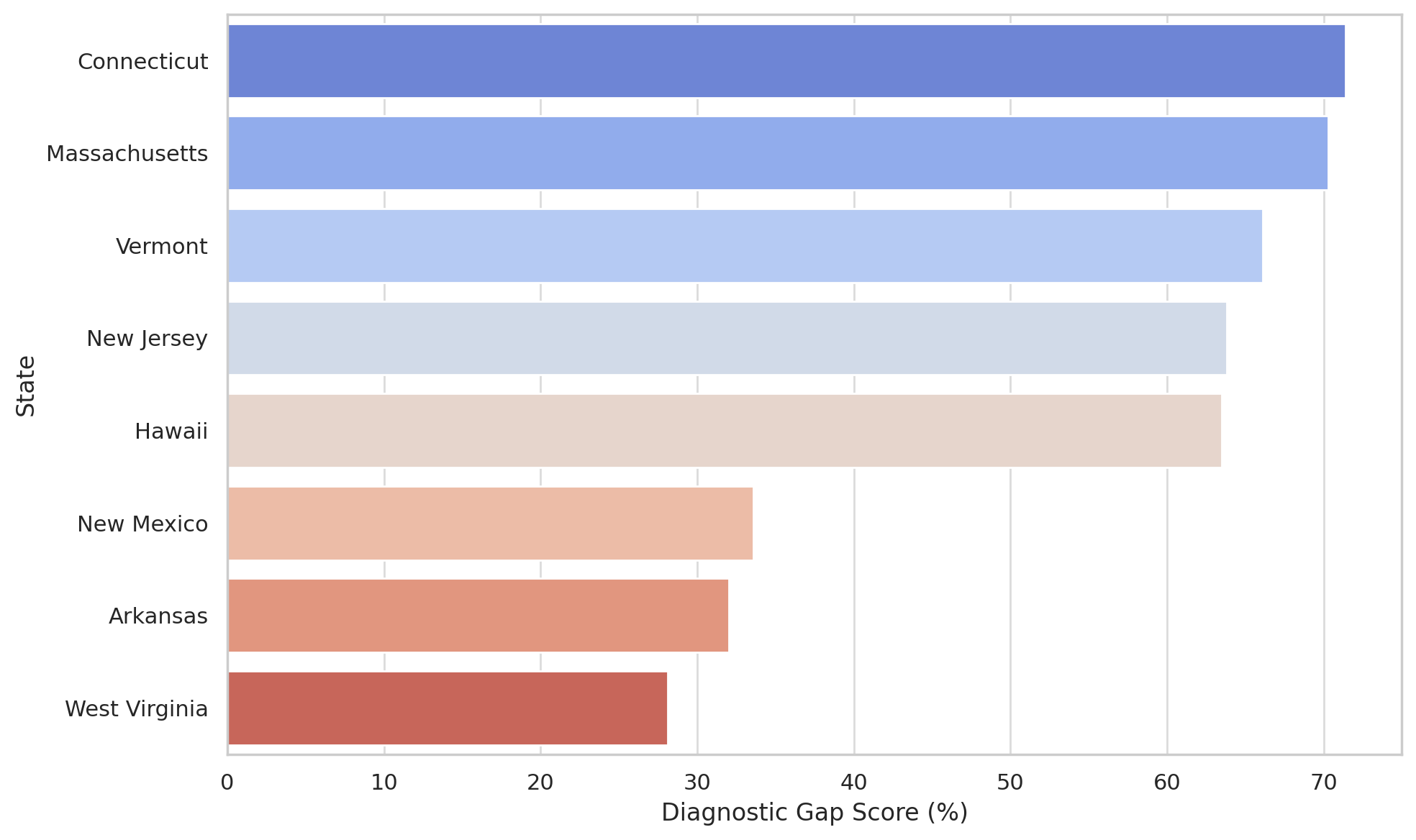
Figure: Figure 1: Adjusted Diagnostic Gap Scores for Selected U.S. States.
States with the highest scores (Connecticut, Massachusetts, Vermont, New Jersey, and Hawaii) demonstrate disproportionately high pancreatic cancer mortality relative to diabetes mortality and pancreatitis prevalence, indicating potential underdiagnosis of type 3c diabetes. In contrast, West Virginia, Arkansas, and New Mexico show lower gap scores, suggesting better recognition and diagnostic alignment. Scores are rounded to match values reported in the abstract.
Disclosures:
John Appiah indicated no relevant financial relationships.
Ewurabena Plange-Kaye indicated no relevant financial relationships.
Chukwunonso Ubanatu indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Emmanuel Asare indicated no relevant financial relationships.
John K. Appiah, MD1, Ewurabena N. Plange-Kaye, DDS2, Chukwunonso Ubanatu, MD1, George S. Blewusi, MD3, Emmanuel Asare, 4. P0024 - Mapping Hidden Type 3c Diabetes Across the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
