Sunday Poster Session
Category: Biliary/Pancreas
P0021 - Characteristics of Early-Onset vs Late-Onset Pancreatic Ductal Adenocarcinoma: A Single-Center Retrospective Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Madeleine Ziqi Wong, MD (she/her/hers)
Stony Brook University Hospital
Stony Brook, NY
Presenting Author(s)
Madeleine Ziqi. Wong, MD1, Kazi Ullah, MD1, Alexandra Rusz, MD2, Mina Zheng, DO3, Lionel D'Souza, MD4
1Stony Brook University Hospital, Stony Brook, NY; 2Renaissance School of Medicine, Stony Brook University, Stony Brook, NY; 3Renaissance School of Medicine at Stony Brook University, Stony Brook, NY; 4Mount Sinai Hospital, New York, NY
Introduction: Studies from the SEER registry have indicated a rise in pancreatic ductal adenocarcinoma (PDAC) cases among individuals under 60 years of age in recent years. Early-onset PDAC has been linked to family history of pancreatic cancer, metabolic syndrome, smoking, pancreatitis, and germline mutations. However, risk factors contributing to early presentation remain poorly defined. We aim to analyze clinicopathological/demographic differences in early diagnosis of PDAC (defined as age ≤ 60 years) vs. a late diagnosis (defined as age > 60 years).
Methods: Clinicopathological/demographic data was retrospectively collected from patients diagnosed with pancreatic neoplasms at our tertiary-care center from 2014 to 2023. MRNs were extracted via TriNetX and de-identified under IRB approval. Patients without PDAC or staging were excluded. Statistical analysis was performed using SPSS v29.0. Univariate analyses compared baseline characteristics. Survival was assessed via Kaplan-Meier and compared via log-rank test. Hazard function illustrated time-dependent risk. Variables associated with survival (p < 0.25) in univariate cox regression were included in a multivariate Cox proportional hazards model to estimate adjusted hazard ratios.
Results: Of the 133 patients (33 early-age and 100 late-age), the early-age group had higher proportions of male gender (67% vs 51%), Hispanic ethnicity (12% vs 0%), family history of pancreatic cancer (15% vs 8%), and chemotherapy treatment (79% vs 66%). The late-age group had higher proportions of Black patients (13% vs 6%), metabolic syndrome (68% vs 30%), prior cancer diagnosis (30% vs 6%), and body-of-pancreas tumors (78% vs 42%). Although median survival was higher in the late-age group (25 vs 20 months), Kaplan-Meier analysis showed better overall survival probabilities in early-age patients (p = 0.431). The hazard function and ratio (0.832, p = 0.506) demonstrated that late-age patients had higher instantaneous risk of death.
Discussion: Clinical and demographic differences suggest a potential genetic or ethnic predisposition to PDAC in younger patients, who were also more likely to receive chemotherapy. In contrast, later diagnosis may reflect cumulative exposures or delayed detection. Although older patients showed slightly longer median survival, overall survival favored the younger cohort. The study is limited by small sample size; ongoing retrospective review of over 2,000 additional patients is planned to enhance statistical power in future analyses.
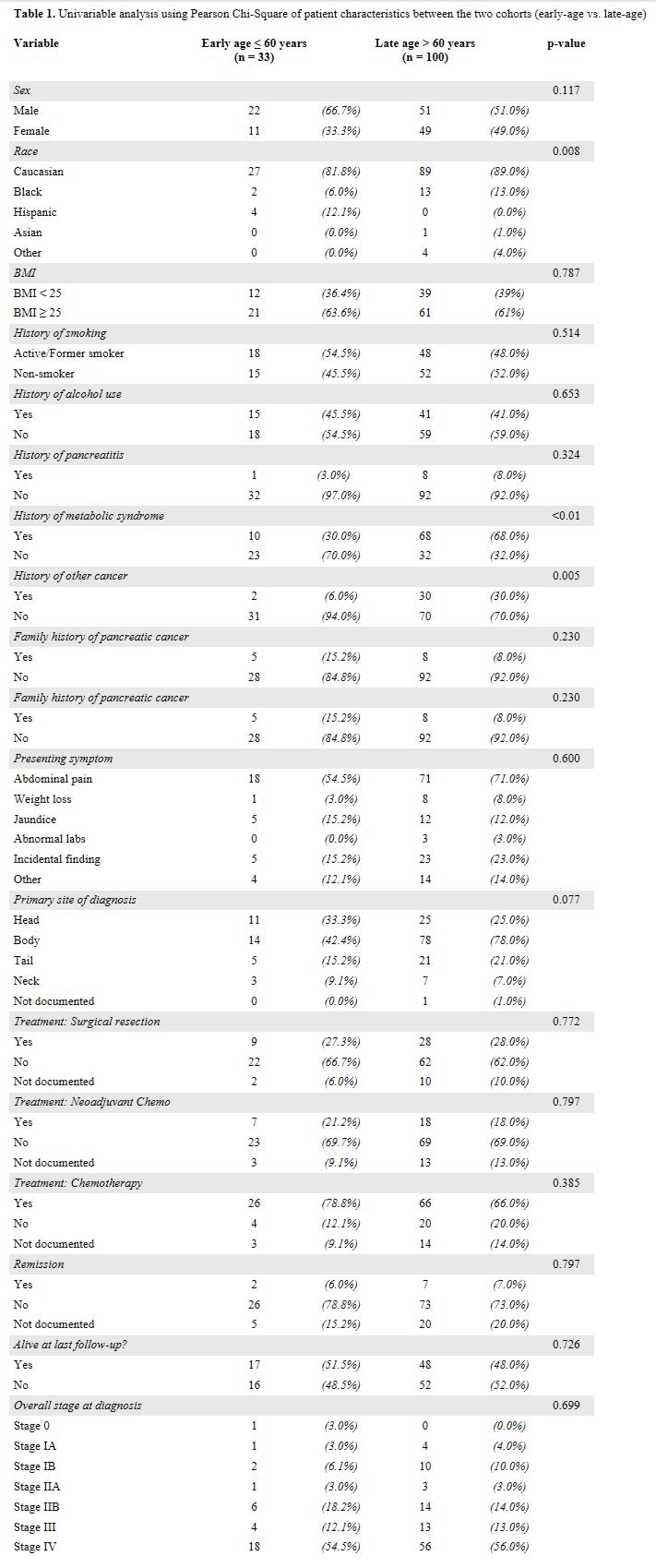
Figure: Table 1. Univariable analysis using Pearson Chi-Square of patient characteristics between the two cohorts (early-age vs. late-age)
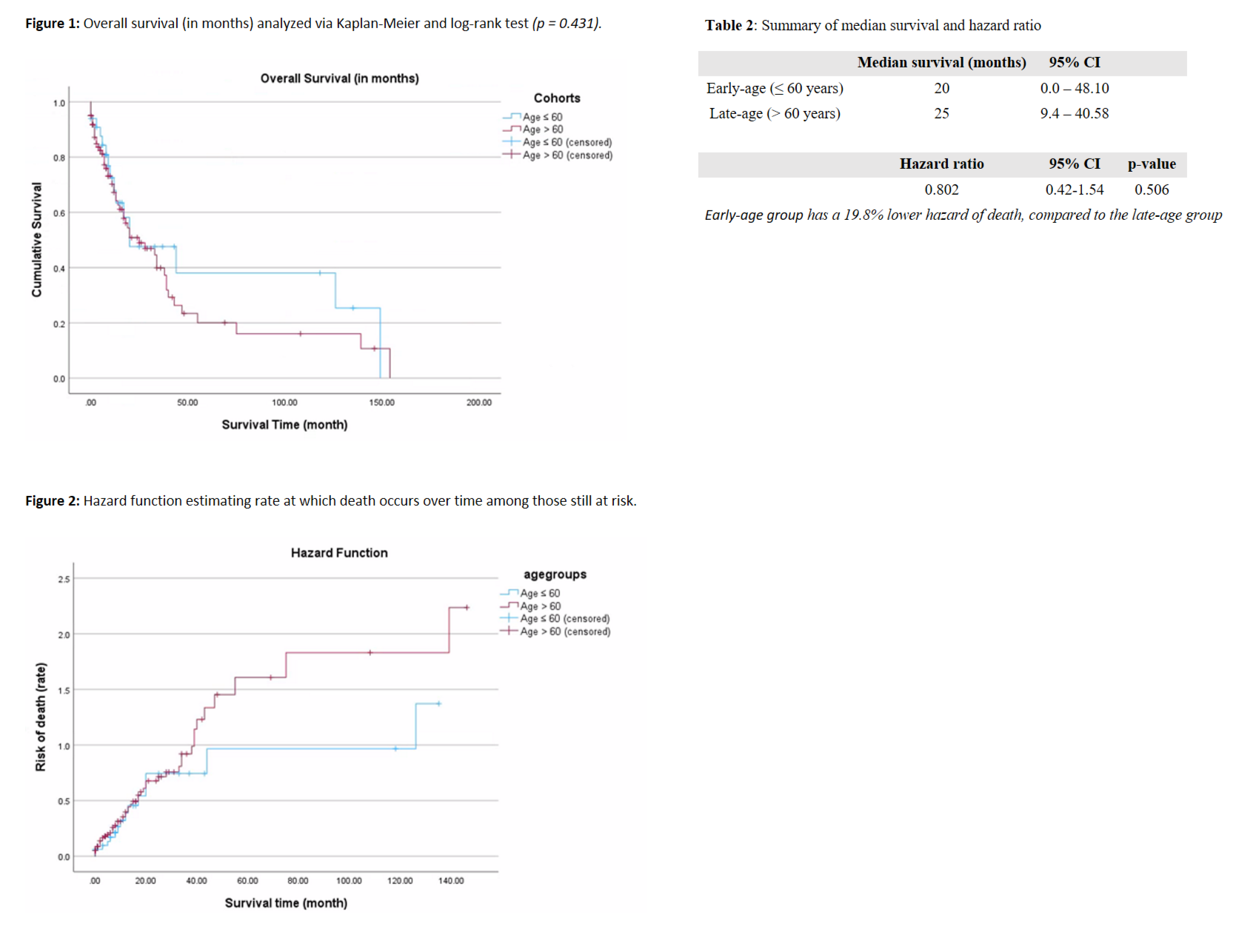
Figure: Figure 1 depicts the overall survival curve (in months) between the two age groups (early-age vs. late-age), analyzed via Kaplan-Meier and compared with log-rank test (p = 0.431). Figure 2 depicts the hazard function which estimates rate at which death occurs over time among those still at risk. Table 2 summarizes the median survival and hazard ratio findings.
Disclosures:
Madeleine Wong indicated no relevant financial relationships.
Kazi Ullah indicated no relevant financial relationships.
Alexandra Rusz indicated no relevant financial relationships.
Mina Zheng indicated no relevant financial relationships.
Lionel D'Souza indicated no relevant financial relationships.
Madeleine Ziqi. Wong, MD1, Kazi Ullah, MD1, Alexandra Rusz, MD2, Mina Zheng, DO3, Lionel D'Souza, MD4. P0021 - Characteristics of Early-Onset vs Late-Onset Pancreatic Ductal Adenocarcinoma: A Single-Center Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stony Brook University Hospital, Stony Brook, NY; 2Renaissance School of Medicine, Stony Brook University, Stony Brook, NY; 3Renaissance School of Medicine at Stony Brook University, Stony Brook, NY; 4Mount Sinai Hospital, New York, NY
Introduction: Studies from the SEER registry have indicated a rise in pancreatic ductal adenocarcinoma (PDAC) cases among individuals under 60 years of age in recent years. Early-onset PDAC has been linked to family history of pancreatic cancer, metabolic syndrome, smoking, pancreatitis, and germline mutations. However, risk factors contributing to early presentation remain poorly defined. We aim to analyze clinicopathological/demographic differences in early diagnosis of PDAC (defined as age ≤ 60 years) vs. a late diagnosis (defined as age > 60 years).
Methods: Clinicopathological/demographic data was retrospectively collected from patients diagnosed with pancreatic neoplasms at our tertiary-care center from 2014 to 2023. MRNs were extracted via TriNetX and de-identified under IRB approval. Patients without PDAC or staging were excluded. Statistical analysis was performed using SPSS v29.0. Univariate analyses compared baseline characteristics. Survival was assessed via Kaplan-Meier and compared via log-rank test. Hazard function illustrated time-dependent risk. Variables associated with survival (p < 0.25) in univariate cox regression were included in a multivariate Cox proportional hazards model to estimate adjusted hazard ratios.
Results: Of the 133 patients (33 early-age and 100 late-age), the early-age group had higher proportions of male gender (67% vs 51%), Hispanic ethnicity (12% vs 0%), family history of pancreatic cancer (15% vs 8%), and chemotherapy treatment (79% vs 66%). The late-age group had higher proportions of Black patients (13% vs 6%), metabolic syndrome (68% vs 30%), prior cancer diagnosis (30% vs 6%), and body-of-pancreas tumors (78% vs 42%). Although median survival was higher in the late-age group (25 vs 20 months), Kaplan-Meier analysis showed better overall survival probabilities in early-age patients (p = 0.431). The hazard function and ratio (0.832, p = 0.506) demonstrated that late-age patients had higher instantaneous risk of death.
Discussion: Clinical and demographic differences suggest a potential genetic or ethnic predisposition to PDAC in younger patients, who were also more likely to receive chemotherapy. In contrast, later diagnosis may reflect cumulative exposures or delayed detection. Although older patients showed slightly longer median survival, overall survival favored the younger cohort. The study is limited by small sample size; ongoing retrospective review of over 2,000 additional patients is planned to enhance statistical power in future analyses.
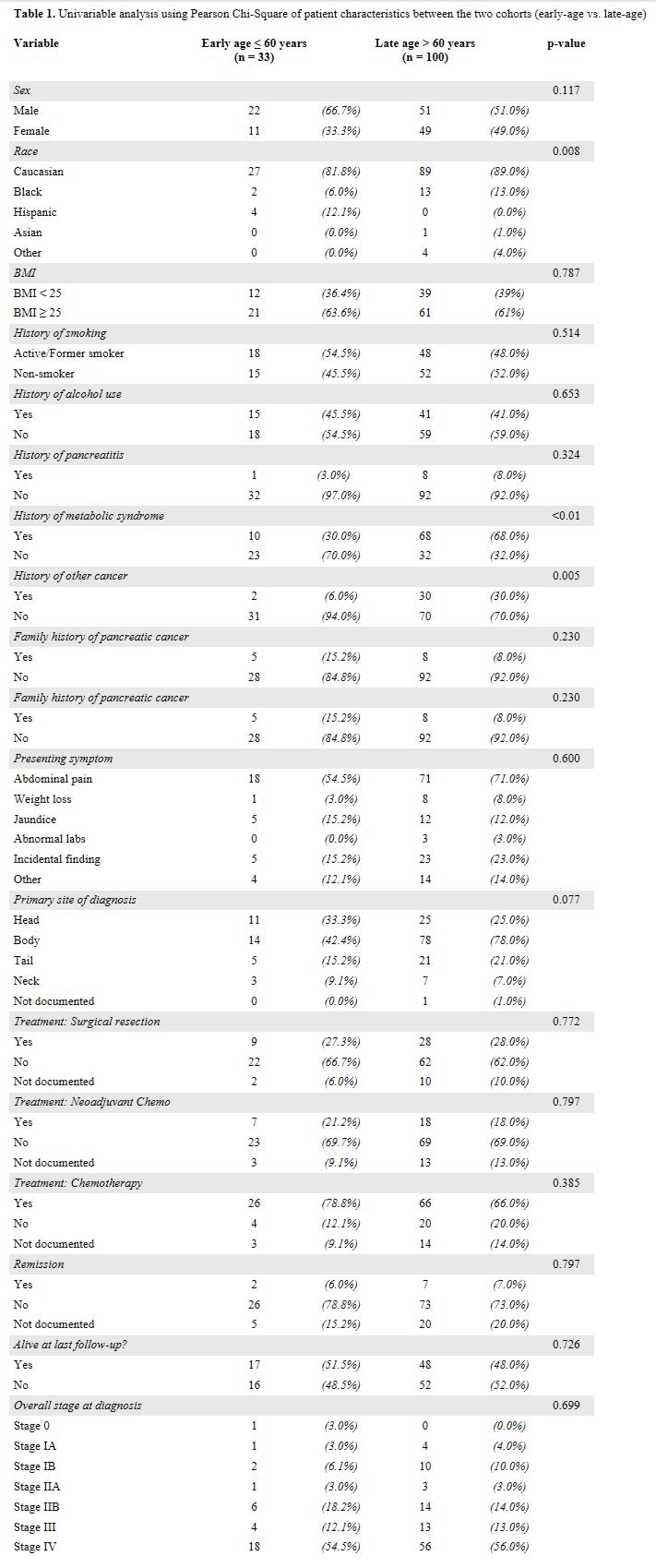
Figure: Table 1. Univariable analysis using Pearson Chi-Square of patient characteristics between the two cohorts (early-age vs. late-age)
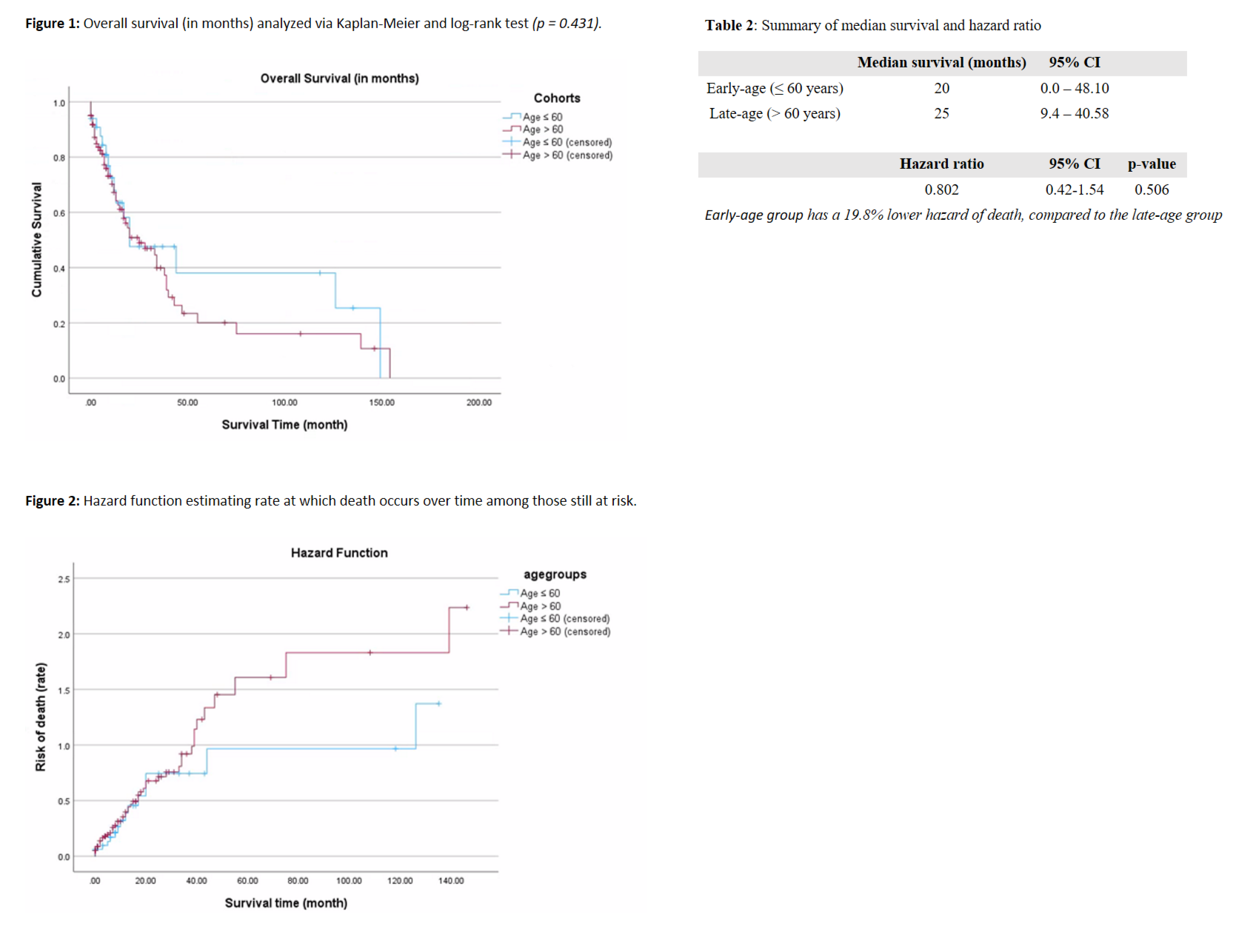
Figure: Figure 1 depicts the overall survival curve (in months) between the two age groups (early-age vs. late-age), analyzed via Kaplan-Meier and compared with log-rank test (p = 0.431). Figure 2 depicts the hazard function which estimates rate at which death occurs over time among those still at risk. Table 2 summarizes the median survival and hazard ratio findings.
Disclosures:
Madeleine Wong indicated no relevant financial relationships.
Kazi Ullah indicated no relevant financial relationships.
Alexandra Rusz indicated no relevant financial relationships.
Mina Zheng indicated no relevant financial relationships.
Lionel D'Souza indicated no relevant financial relationships.
Madeleine Ziqi. Wong, MD1, Kazi Ullah, MD1, Alexandra Rusz, MD2, Mina Zheng, DO3, Lionel D'Souza, MD4. P0021 - Characteristics of Early-Onset vs Late-Onset Pancreatic Ductal Adenocarcinoma: A Single-Center Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
