Sunday Poster Session
Category: Biliary/Pancreas
P0014 - Compounded Disease Burden in Chronic Pancreatitis Patients With HIV: A Propensity-Matched Nationwide Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AI
AbdiGhani Ismail, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
AbdiGhani Ismail, MD1, Adel Hajj Ali, MD1, Saad Saadat, MD1, Azizullah Beran, MD1, Indira Bhavsar-Burke, MD2, John Guardiola, MD1, Nasir Saleem, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2University of Texas Southwestern School of Medicine, Dallas, TX
Introduction: Chronic pancreatitis (CP) is a debilitating condition characterized by progressive inflammation and fibrosis of the pancreas. While CP has been extensively studied, limited data exist on outcomes in patients who have both CP and human immunodeficiency virus (HIV). Given the chronic inflammatory and systemic effects of HIV, we hypothesized that coexisting HIV may be associated with worse clinical outcomes in CP patients.
Methods: We conducted a retrospective cohort study using the TriNetX database through May 29, 2025, identifying adult patients diagnosed with both chronic pancreatitis (CP) and HIV. Patients with a prior diagnosis of pancreatic malignancy, solid organ transplant, or cystic fibrosis were excluded. Two cohorts were created: those with CP and HIV (CP+HIV) and those with CP alone. Propensity score matching (1:1) was performed using 38 covariates, including demographic characteristics and comorbidities. The index event for the CP+HIV group was the diagnosis of HIV; any outcomes occurring prior to this index event were excluded. Primary outcomes included risk differences in malnutrition, total parenteral nutrition use, hospitalizations, and mortality.
Results: After propensity score matching, there were a total of 2131 patients in the CP+HIV cohort, and 2131 patients in the CP only cohort. There were no significant demographic differences after PS matching. Patients identified with concurrent HIV and CP <were found to have a significant increased risk difference for diagnoses of malnutrition, low BMI, development of mood disorder, heart disease, diabetes, and mortality. Subgroup analysis for this population based on CD4 was limited by sample size, but even in patients with a CD4 count greater than 200, there was statistically significant increased risk for mood disorder development and heart disease. There was no significant difference in pancreatic enzyme replacement therapy between the groups.
Discussion: Patients with concurrent CP and HIV experience significantly worse clinical outcomes, including higher rates of malnutrition, psychiatric comorbidity, cirrhosis, hospitalization, and mortality compared to CP-only patients. Subgroup analysis of patients with CD4 >200 showed attenuation of most adverse outcomes, suggesting immune status may influence risk severity, however this sample size was small. These findings underscore the need for targeted screening and multidisciplinary management strategies for this vulnerable population.
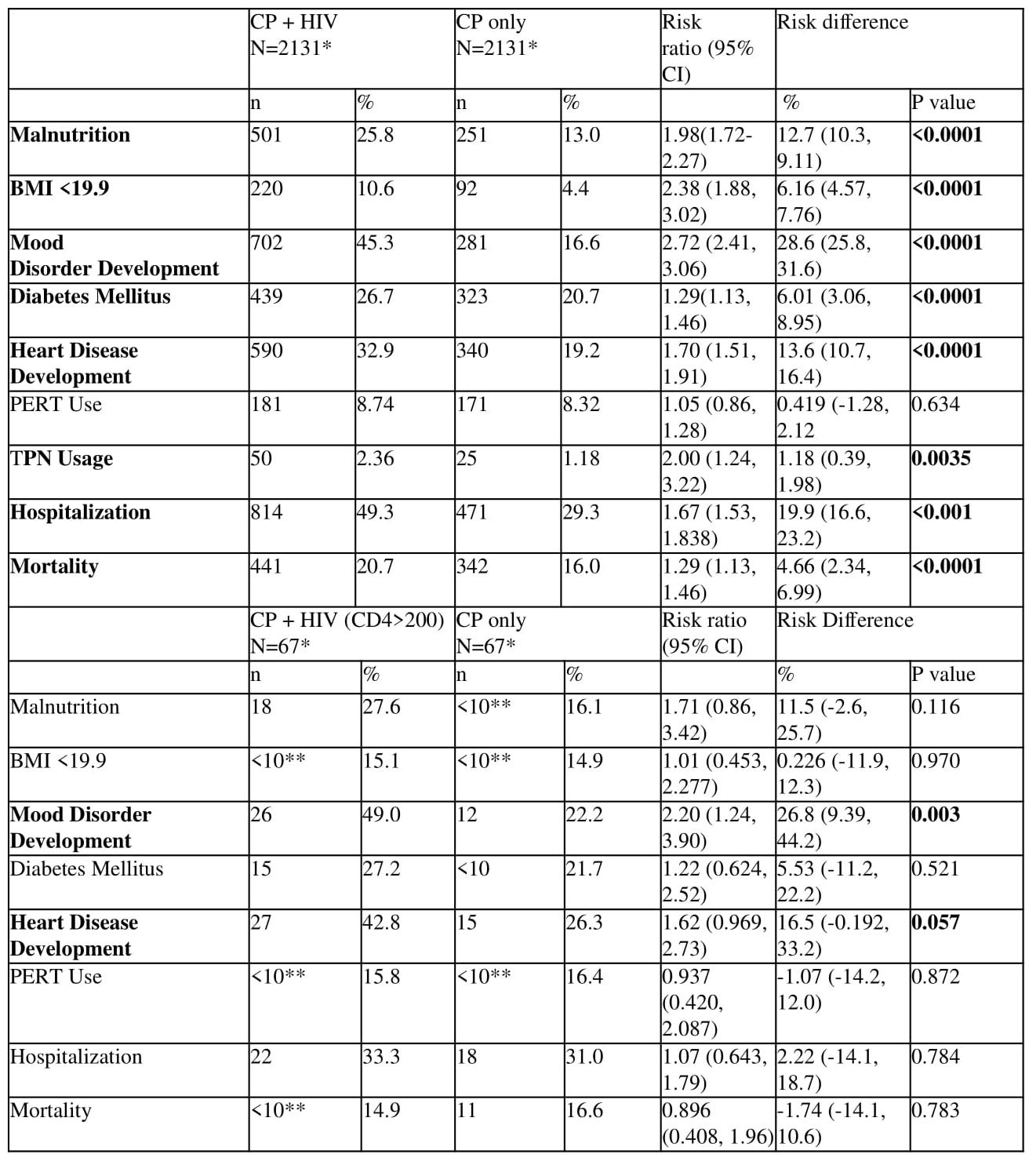
Figure: Table 1: Outcomes of patients with CP + HIV compared to patients with CP Only
*Certain cohort patients with outcomes prior to index event were excluded from results
**TriNetX database did not give numerical value if N <10 in order to protect patient privacy
Disclosures:
AbdiGhani Ismail indicated no relevant financial relationships.
Adel Hajj Ali indicated no relevant financial relationships.
Saad Saadat indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Guardiola indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
AbdiGhani Ismail, MD1, Adel Hajj Ali, MD1, Saad Saadat, MD1, Azizullah Beran, MD1, Indira Bhavsar-Burke, MD2, John Guardiola, MD1, Nasir Saleem, MD1. P0014 - Compounded Disease Burden in Chronic Pancreatitis Patients With HIV: A Propensity-Matched Nationwide Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2University of Texas Southwestern School of Medicine, Dallas, TX
Introduction: Chronic pancreatitis (CP) is a debilitating condition characterized by progressive inflammation and fibrosis of the pancreas. While CP has been extensively studied, limited data exist on outcomes in patients who have both CP and human immunodeficiency virus (HIV). Given the chronic inflammatory and systemic effects of HIV, we hypothesized that coexisting HIV may be associated with worse clinical outcomes in CP patients.
Methods: We conducted a retrospective cohort study using the TriNetX database through May 29, 2025, identifying adult patients diagnosed with both chronic pancreatitis (CP) and HIV. Patients with a prior diagnosis of pancreatic malignancy, solid organ transplant, or cystic fibrosis were excluded. Two cohorts were created: those with CP and HIV (CP+HIV) and those with CP alone. Propensity score matching (1:1) was performed using 38 covariates, including demographic characteristics and comorbidities. The index event for the CP+HIV group was the diagnosis of HIV; any outcomes occurring prior to this index event were excluded. Primary outcomes included risk differences in malnutrition, total parenteral nutrition use, hospitalizations, and mortality.
Results: After propensity score matching, there were a total of 2131 patients in the CP+HIV cohort, and 2131 patients in the CP only cohort. There were no significant demographic differences after PS matching. Patients identified with concurrent HIV and CP <were found to have a significant increased risk difference for diagnoses of malnutrition, low BMI, development of mood disorder, heart disease, diabetes, and mortality. Subgroup analysis for this population based on CD4 was limited by sample size, but even in patients with a CD4 count greater than 200, there was statistically significant increased risk for mood disorder development and heart disease. There was no significant difference in pancreatic enzyme replacement therapy between the groups.
Discussion: Patients with concurrent CP and HIV experience significantly worse clinical outcomes, including higher rates of malnutrition, psychiatric comorbidity, cirrhosis, hospitalization, and mortality compared to CP-only patients. Subgroup analysis of patients with CD4 >200 showed attenuation of most adverse outcomes, suggesting immune status may influence risk severity, however this sample size was small. These findings underscore the need for targeted screening and multidisciplinary management strategies for this vulnerable population.
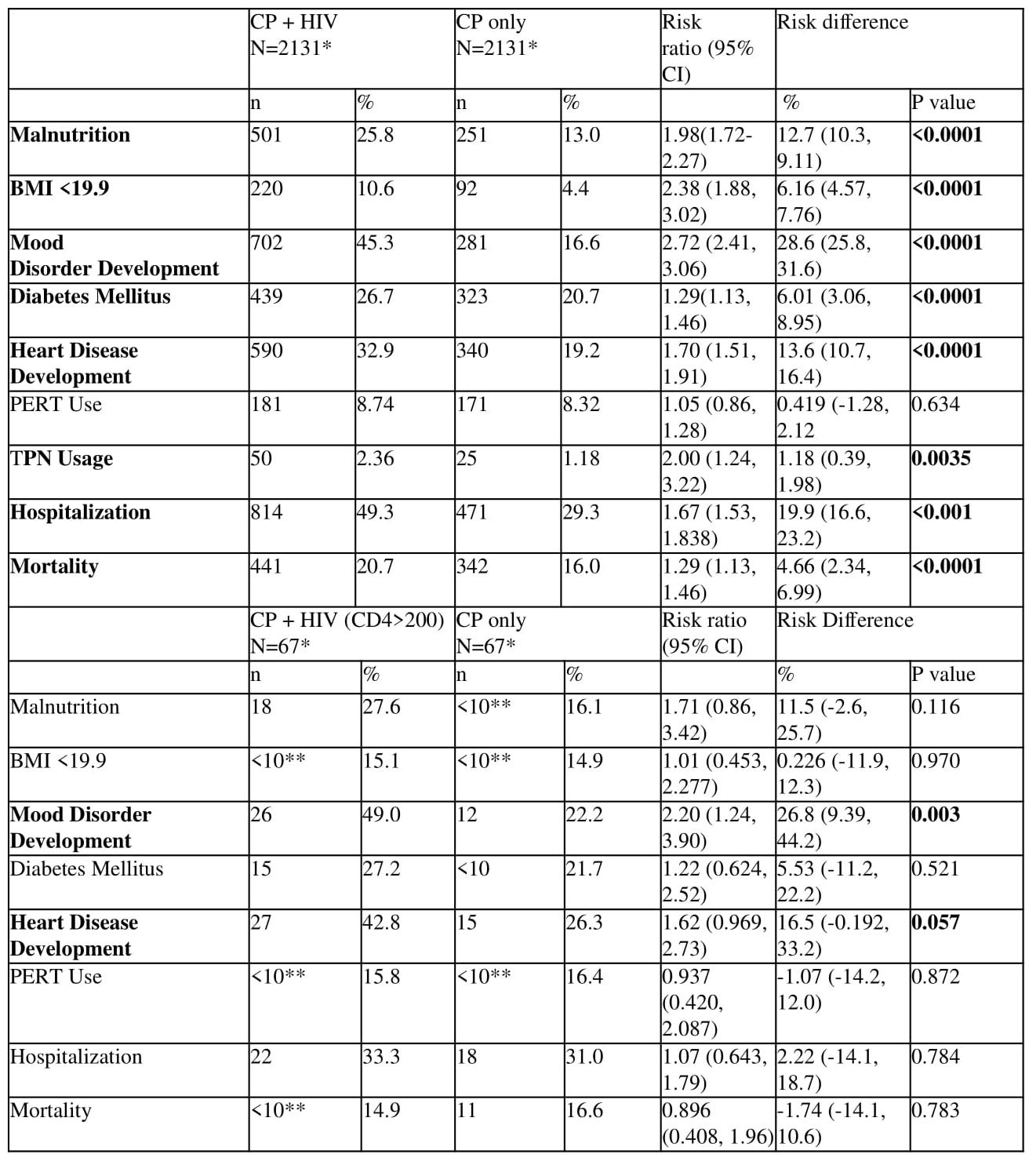
Figure: Table 1: Outcomes of patients with CP + HIV compared to patients with CP Only
*Certain cohort patients with outcomes prior to index event were excluded from results
**TriNetX database did not give numerical value if N <10 in order to protect patient privacy
Disclosures:
AbdiGhani Ismail indicated no relevant financial relationships.
Adel Hajj Ali indicated no relevant financial relationships.
Saad Saadat indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Guardiola indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
AbdiGhani Ismail, MD1, Adel Hajj Ali, MD1, Saad Saadat, MD1, Azizullah Beran, MD1, Indira Bhavsar-Burke, MD2, John Guardiola, MD1, Nasir Saleem, MD1. P0014 - Compounded Disease Burden in Chronic Pancreatitis Patients With HIV: A Propensity-Matched Nationwide Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
