Sunday Poster Session
Category: Biliary/Pancreas
P0009 - Incremental Value of Endoscopic Ultrasound for Asymptomatic Pancreatic Cysts 20-30 mm in Size on Cross-Sectional Imaging
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KG
Kanika Garg, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Kanika Garg, MD, Agnieszka Maniak, MD, Thomas J. Wang, MD, Matthew Eganhouse, MD, Christopher Babiarz, MD, Christopher G. Chapman, MD, Neal A. Mehta, MD, Irving Waxman, MD, FACG, Ajaypal Singh, MD
Rush University Medical Center, Chicago, IL
Introduction: Pancreatic cysts are commonly diagnosed incidentally and often require long-term surveillance. For presumed mucinous cysts measuring 20-30mm, both endoscopic ultrasound (EUS) and magnetic resonance imaging (MRI) are recommended at 6-month intervals per guidelines. Despite its invasiveness, risks, and cost, EUS impact on management vs MRI alone remains unclear. We aimed to assess EUS utility for asymptomatic pancreatic cysts 20-30mm in size and its impact on surveillance decisions.
Methods: This single-center retrospective study included patients with pancreatic cysts measuring 20-30 mm on cross-sectional imaging (CSI) who underwent EUS between 2018-2024. Cysts with interval increase in size but still < 3 cm on CSI were also included. Patients were excluded if initial imaging showed pancreatic duct dilation ( >5mm) or mural nodules. Interval growth was defined as cyst growth >2.5 mm/year. Clinical risk factors included new-onset diabetes within one year, acute pancreatitis, or 1st-degree relative with pancreatic cancer. Primary outcome was change in management following EUS. Patients were stratified by interval growth and clinical risk factors.
Results: Of 103 patients (mean age 68±12.7 years, 57.3% female), EUS led to management changes in 7 patients (6.8%): 4 had shortened surveillance intervals and 3 were referred for surgery. Among 40 patients (38.8%) with interval cyst growth >2.5 mm/year, 5 (12.5%) had management changes: 4 had shortened surveillance and 1 was referred for surgery. Of the 63 patients without growth, 12 (19.0%) had clinical risk factors, 2 of which were referred for surgery. The remaining 51 patients without interval growth or clinical risk factors had no management escalation. Notably, 5 patients (9.8%) in this low-risk group had surveillance discontinued after EUS diagnosis of serous cystadenoma. Patients with interval growth or clinical risk factors were significantly more likely to have management changes compared to those without (10.9% vs 0%, p=0.0126).
Discussion: EUS provides incremental clinical value in selected patients with 20-30 mm pancreatic cysts, leading to management changes in ~7% overall. Patients without interval growth or clinical risk factors derived no benefit from EUS for escalating surveillance or surgical referral, though some benefited from surveillance de-escalation. These findings support a risk-stratified approach where EUS may be deferred in truly low-risk patients, potentially reducing costs and patient burden while maintaining safety.
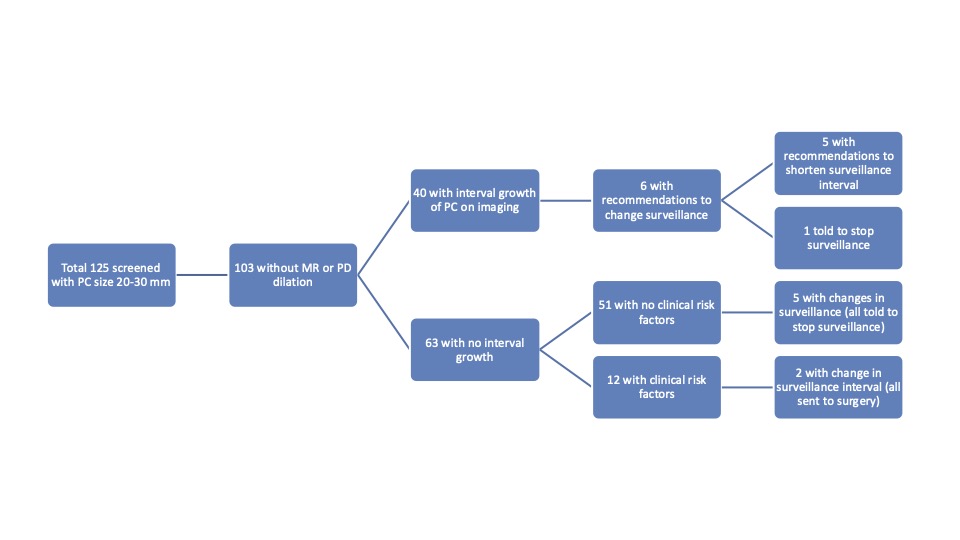
Figure: EUS outcomes stratified by interval growth and clinical risk factor (PC = pancreatic cyst; MR = mural nodule; PD = pancreatic duct)
Disclosures:
Kanika Garg indicated no relevant financial relationships.
Agnieszka Maniak indicated no relevant financial relationships.
Thomas Wang indicated no relevant financial relationships.
Matthew Eganhouse indicated no relevant financial relationships.
Christopher Babiarz indicated no relevant financial relationships.
Christopher Chapman: Boston Scientific – Consultant. Olympus – Consultant. Phathom Pharmaceuticals – Consultant.
Neal Mehta: Boston Scientific – Consultant. Castle Biosciences – Consultant. ConMed – Consultant. Medtronic – Consultant. Olympus – Consultant.
Irving Waxman: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic – Consultant.
Ajaypal Singh: Boston Scientific – Consultant. Creo – Consultant. Olympus – Consultant.
Kanika Garg, MD, Agnieszka Maniak, MD, Thomas J. Wang, MD, Matthew Eganhouse, MD, Christopher Babiarz, MD, Christopher G. Chapman, MD, Neal A. Mehta, MD, Irving Waxman, MD, FACG, Ajaypal Singh, MD. P0009 - Incremental Value of Endoscopic Ultrasound for Asymptomatic Pancreatic Cysts 20-30 mm in Size on Cross-Sectional Imaging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Pancreatic cysts are commonly diagnosed incidentally and often require long-term surveillance. For presumed mucinous cysts measuring 20-30mm, both endoscopic ultrasound (EUS) and magnetic resonance imaging (MRI) are recommended at 6-month intervals per guidelines. Despite its invasiveness, risks, and cost, EUS impact on management vs MRI alone remains unclear. We aimed to assess EUS utility for asymptomatic pancreatic cysts 20-30mm in size and its impact on surveillance decisions.
Methods: This single-center retrospective study included patients with pancreatic cysts measuring 20-30 mm on cross-sectional imaging (CSI) who underwent EUS between 2018-2024. Cysts with interval increase in size but still < 3 cm on CSI were also included. Patients were excluded if initial imaging showed pancreatic duct dilation ( >5mm) or mural nodules. Interval growth was defined as cyst growth >2.5 mm/year. Clinical risk factors included new-onset diabetes within one year, acute pancreatitis, or 1st-degree relative with pancreatic cancer. Primary outcome was change in management following EUS. Patients were stratified by interval growth and clinical risk factors.
Results: Of 103 patients (mean age 68±12.7 years, 57.3% female), EUS led to management changes in 7 patients (6.8%): 4 had shortened surveillance intervals and 3 were referred for surgery. Among 40 patients (38.8%) with interval cyst growth >2.5 mm/year, 5 (12.5%) had management changes: 4 had shortened surveillance and 1 was referred for surgery. Of the 63 patients without growth, 12 (19.0%) had clinical risk factors, 2 of which were referred for surgery. The remaining 51 patients without interval growth or clinical risk factors had no management escalation. Notably, 5 patients (9.8%) in this low-risk group had surveillance discontinued after EUS diagnosis of serous cystadenoma. Patients with interval growth or clinical risk factors were significantly more likely to have management changes compared to those without (10.9% vs 0%, p=0.0126).
Discussion: EUS provides incremental clinical value in selected patients with 20-30 mm pancreatic cysts, leading to management changes in ~7% overall. Patients without interval growth or clinical risk factors derived no benefit from EUS for escalating surveillance or surgical referral, though some benefited from surveillance de-escalation. These findings support a risk-stratified approach where EUS may be deferred in truly low-risk patients, potentially reducing costs and patient burden while maintaining safety.
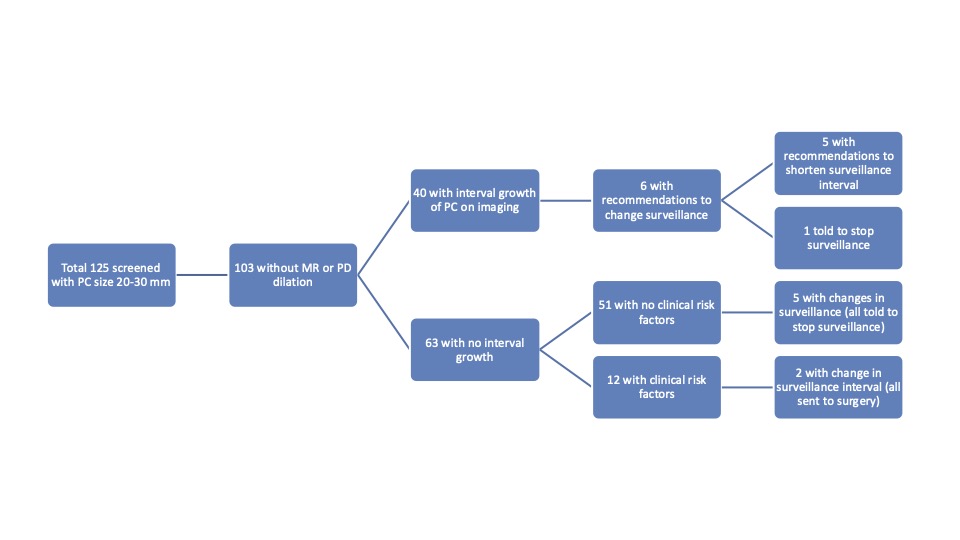
Figure: EUS outcomes stratified by interval growth and clinical risk factor (PC = pancreatic cyst; MR = mural nodule; PD = pancreatic duct)
Disclosures:
Kanika Garg indicated no relevant financial relationships.
Agnieszka Maniak indicated no relevant financial relationships.
Thomas Wang indicated no relevant financial relationships.
Matthew Eganhouse indicated no relevant financial relationships.
Christopher Babiarz indicated no relevant financial relationships.
Christopher Chapman: Boston Scientific – Consultant. Olympus – Consultant. Phathom Pharmaceuticals – Consultant.
Neal Mehta: Boston Scientific – Consultant. Castle Biosciences – Consultant. ConMed – Consultant. Medtronic – Consultant. Olympus – Consultant.
Irving Waxman: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic – Consultant.
Ajaypal Singh: Boston Scientific – Consultant. Creo – Consultant. Olympus – Consultant.
Kanika Garg, MD, Agnieszka Maniak, MD, Thomas J. Wang, MD, Matthew Eganhouse, MD, Christopher Babiarz, MD, Christopher G. Chapman, MD, Neal A. Mehta, MD, Irving Waxman, MD, FACG, Ajaypal Singh, MD. P0009 - Incremental Value of Endoscopic Ultrasound for Asymptomatic Pancreatic Cysts 20-30 mm in Size on Cross-Sectional Imaging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
