Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3A: Liver / Functional
43 - Neuroimaging in Veterans With Irritable Bowel Syndrome (IBS): Analysis of the TRACTS (Translational Research Center for Traumatic Brain Injury and Stress Disorders) Longitudinal Prospective Cohort Study
Tuesday, October 28, 2025
3:15 PM - 3:25 PM PDT
Location: North Ballroom 120D
Marisa Wu, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Marisa Wu, MD1, Jacqueline Liu, MD1, Rosa L. Yu, MD1, Tyler Robinson, PhD2, Kathleen Cheng, MD1, Jack Carbaugh, MS2, Catherine Fortier, PhD2, William Milberg, PhD2, David Salat, PhD2, Horst C. Weber, MD2
1Boston Medical Center, Boston, MA; 2VA Boston Healthcare System, Jamaica Plain, MA
Introduction: IBS is a highly prevalent disorder of gut-brain interaction that is frequently comorbid with PTSD. Prior studies in non-veterans with IBS suggest that the brain areas involved are associated with pain or emotional processing and visceral sensation, but studies in the veteran population are lacking. This study aims to identify structural and functional brain changes in veterans with IBS, with or without PTSD, to gain insight into the pathophysiology of IBS.
Methods: This study includes veterans enrolled in TRACTS, where participants undergo neuropsychiatric assessments and neuroimaging with MRI. Participants screened in for IBS through review of the electronic health record based on Rome IV criteria. Exclusion criteria included inflammatory bowel conditions prior colonic surgery, and incomplete baseline data. Functional connectivity was modeled using a seed-based correlation approach focused on eight components of the default mode network (DMN). Linear regression controlling for PTSD was used to estimate the effect of IBS on various brain regions. Data processing of major MRI sequences was used to measure morphometric properties of cortical and subcortical gray matter to obtain structural characteristics. Two-sample T tests were used to generate pairwise comparisons between groups. P< 0.05 was considered significant.
Results: A total of 587 participants were enrolled including 50 IBS patients. Demographic characteristics are shown in Table 1. When controlling for PTSD, functional MRI showed higher connectivity between the cingulate and the bitemporal components of the DMN associated with IBS (Table 2). The DMN plays a key role in self-referential processing and emotional regulation. Structural data showed differences between participants with IBS and those with PTSD only. The structural findings were distinct from the areas noted to have increased functional connectivity in IBS.
Discussion: In this first structural and functional neuroimaging study in a large veteran population with IBS and PTSD, unique structural and functional brain imaging differences were identified in veterans with IBS compared with controls and those with PTSD. These results contrast with prior functional studies which showed reduced temporal lobe activation and resting-state functional connectivity in the DMN in IBS. This might suggest distinct brain pathomechanisms for IBS and PTSD in different brain regions which warrants exploration of their clinical phenotypes.
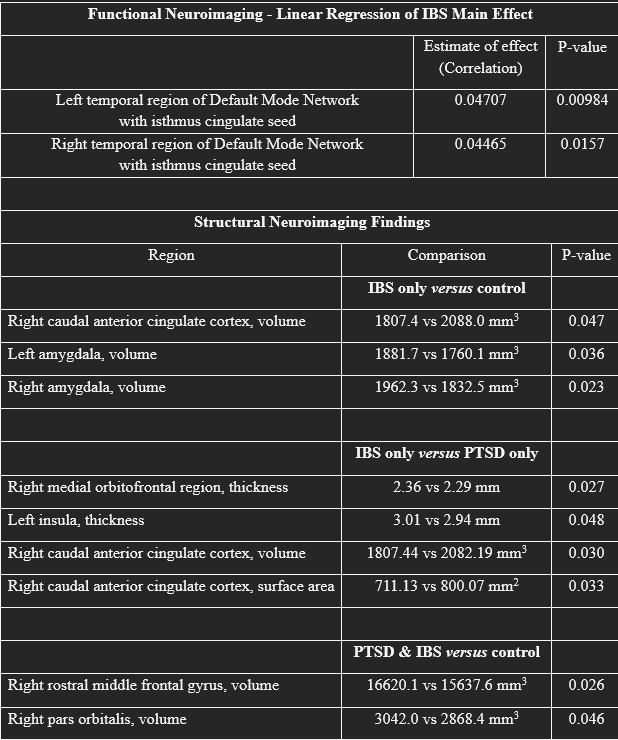
Figure: Table 1: Demographic data of Study Participants in TRACTS:
In a total of 587 participants in TRACTS, 50 were screened in for IBS based on the presence of clinical Rome IV criteria (recurrent abdominal pain associated with a change in bowel habits) and/or ICD10 coding during electronic health record review. Race was self-reported, and the ‘Other’ race category includes individuals who are multi-racial as well as those with not reported race. The majority of participants were White and male. Demographic characteristics were similar between groups except a slightly younger age of participants with IBS. TRACTS, Translational Research Center for Traumatic Brain Injury and Stress Disorders; BMI, Body Mass Index; IBS, Irritable bowel syndrome; PTSD, post-traumatic stress disorder.
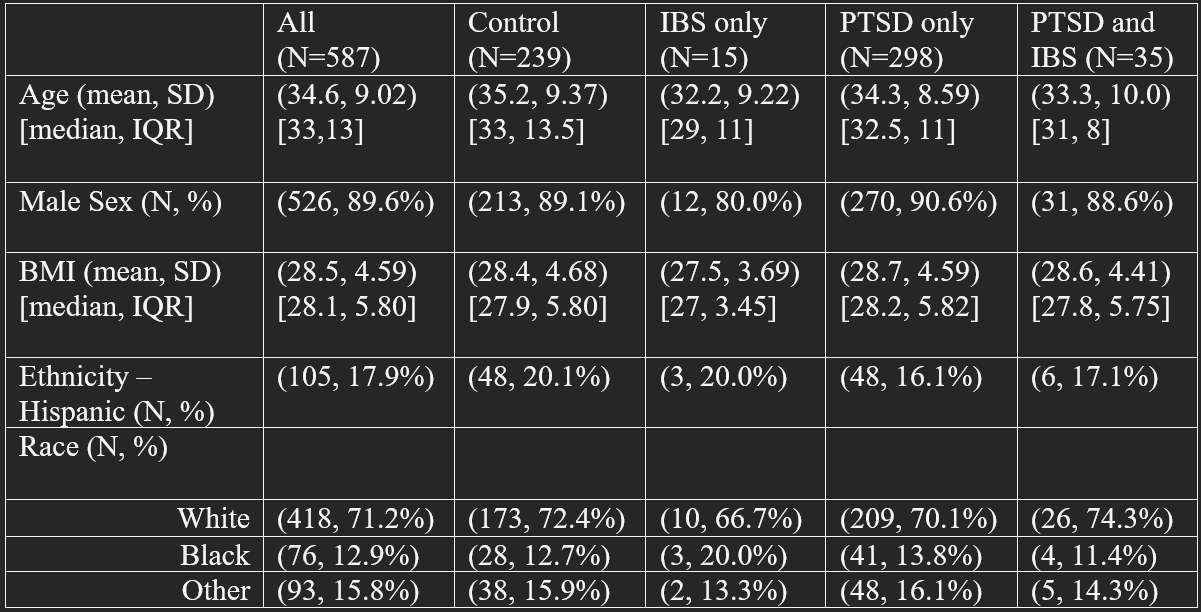
Figure: Table 2: Significant Functional and Structural MRI Neuroimaging Findings:
Regarding the functional MRI cohort (“Functional Neuroimaging “, top), of 587 TRACTS participants, 50 were screened in for IBS through review of the electronic health record based on Rome IV criteria.
Results summarized under “Structural Neuroimaging Findings” (bottom) are based on an earlier analysis of the TRACTS cohort with a smaller sample size (N=499) with 43 IBS participants. No significant differences were noted between the demographic patterns (data not shown).
Disclosures:
Marisa Wu indicated no relevant financial relationships.
Jacqueline Liu indicated no relevant financial relationships.
Rosa Yu indicated no relevant financial relationships.
Tyler Robinson indicated no relevant financial relationships.
Kathleen Cheng indicated no relevant financial relationships.
Jack Carbaugh indicated no relevant financial relationships.
Catherine Fortier indicated no relevant financial relationships.
William Milberg indicated no relevant financial relationships.
David Salat indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Marisa Wu, MD1, Jacqueline Liu, MD1, Rosa L. Yu, MD1, Tyler Robinson, PhD2, Kathleen Cheng, MD1, Jack Carbaugh, MS2, Catherine Fortier, PhD2, William Milberg, PhD2, David Salat, PhD2, Horst C. Weber, MD2, 43, Neuroimaging in Veterans With Irritable Bowel Syndrome (IBS): Analysis of the TRACTS (Translational Research Center for Traumatic Brain Injury and Stress Disorders) Longitudinal Prospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2VA Boston Healthcare System, Jamaica Plain, MA
Introduction: IBS is a highly prevalent disorder of gut-brain interaction that is frequently comorbid with PTSD. Prior studies in non-veterans with IBS suggest that the brain areas involved are associated with pain or emotional processing and visceral sensation, but studies in the veteran population are lacking. This study aims to identify structural and functional brain changes in veterans with IBS, with or without PTSD, to gain insight into the pathophysiology of IBS.
Methods: This study includes veterans enrolled in TRACTS, where participants undergo neuropsychiatric assessments and neuroimaging with MRI. Participants screened in for IBS through review of the electronic health record based on Rome IV criteria. Exclusion criteria included inflammatory bowel conditions prior colonic surgery, and incomplete baseline data. Functional connectivity was modeled using a seed-based correlation approach focused on eight components of the default mode network (DMN). Linear regression controlling for PTSD was used to estimate the effect of IBS on various brain regions. Data processing of major MRI sequences was used to measure morphometric properties of cortical and subcortical gray matter to obtain structural characteristics. Two-sample T tests were used to generate pairwise comparisons between groups. P< 0.05 was considered significant.
Results: A total of 587 participants were enrolled including 50 IBS patients. Demographic characteristics are shown in Table 1. When controlling for PTSD, functional MRI showed higher connectivity between the cingulate and the bitemporal components of the DMN associated with IBS (Table 2). The DMN plays a key role in self-referential processing and emotional regulation. Structural data showed differences between participants with IBS and those with PTSD only. The structural findings were distinct from the areas noted to have increased functional connectivity in IBS.
Discussion: In this first structural and functional neuroimaging study in a large veteran population with IBS and PTSD, unique structural and functional brain imaging differences were identified in veterans with IBS compared with controls and those with PTSD. These results contrast with prior functional studies which showed reduced temporal lobe activation and resting-state functional connectivity in the DMN in IBS. This might suggest distinct brain pathomechanisms for IBS and PTSD in different brain regions which warrants exploration of their clinical phenotypes.
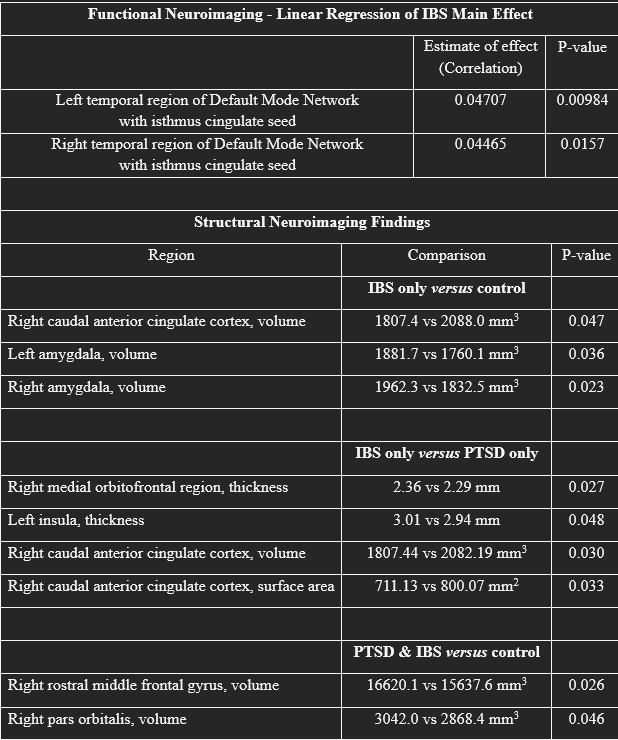
Figure: Table 1: Demographic data of Study Participants in TRACTS:
In a total of 587 participants in TRACTS, 50 were screened in for IBS based on the presence of clinical Rome IV criteria (recurrent abdominal pain associated with a change in bowel habits) and/or ICD10 coding during electronic health record review. Race was self-reported, and the ‘Other’ race category includes individuals who are multi-racial as well as those with not reported race. The majority of participants were White and male. Demographic characteristics were similar between groups except a slightly younger age of participants with IBS. TRACTS, Translational Research Center for Traumatic Brain Injury and Stress Disorders; BMI, Body Mass Index; IBS, Irritable bowel syndrome; PTSD, post-traumatic stress disorder.
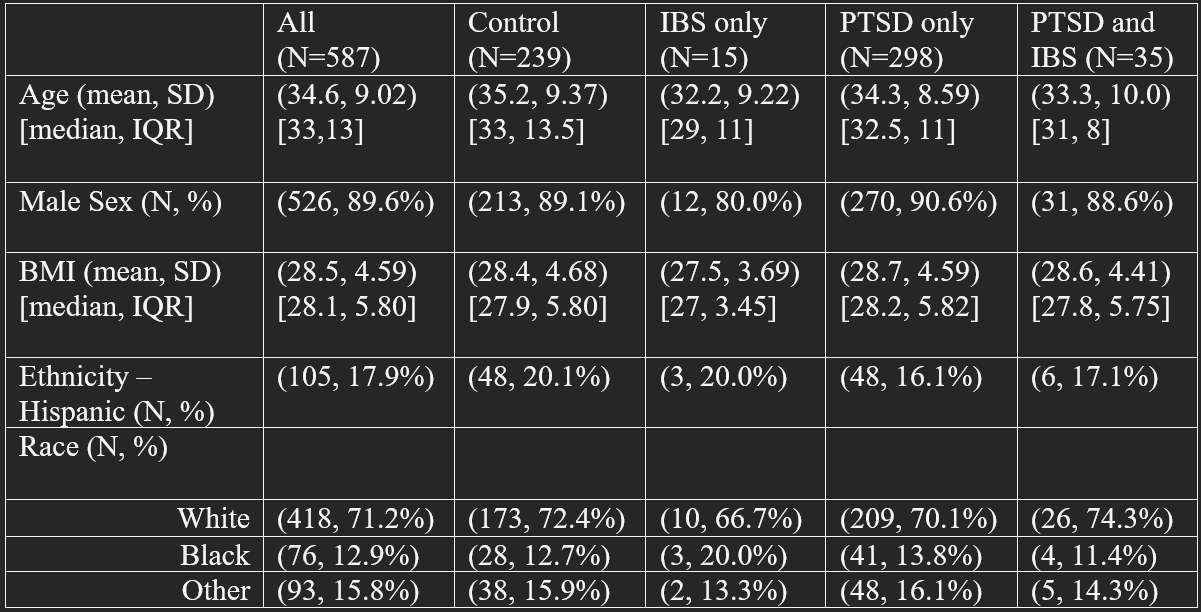
Figure: Table 2: Significant Functional and Structural MRI Neuroimaging Findings:
Regarding the functional MRI cohort (“Functional Neuroimaging “, top), of 587 TRACTS participants, 50 were screened in for IBS through review of the electronic health record based on Rome IV criteria.
Results summarized under “Structural Neuroimaging Findings” (bottom) are based on an earlier analysis of the TRACTS cohort with a smaller sample size (N=499) with 43 IBS participants. No significant differences were noted between the demographic patterns (data not shown).
Disclosures:
Marisa Wu indicated no relevant financial relationships.
Jacqueline Liu indicated no relevant financial relationships.
Rosa Yu indicated no relevant financial relationships.
Tyler Robinson indicated no relevant financial relationships.
Kathleen Cheng indicated no relevant financial relationships.
Jack Carbaugh indicated no relevant financial relationships.
Catherine Fortier indicated no relevant financial relationships.
William Milberg indicated no relevant financial relationships.
David Salat indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Marisa Wu, MD1, Jacqueline Liu, MD1, Rosa L. Yu, MD1, Tyler Robinson, PhD2, Kathleen Cheng, MD1, Jack Carbaugh, MS2, Catherine Fortier, PhD2, William Milberg, PhD2, David Salat, PhD2, Horst C. Weber, MD2, 43, Neuroimaging in Veterans With Irritable Bowel Syndrome (IBS): Analysis of the TRACTS (Translational Research Center for Traumatic Brain Injury and Stress Disorders) Longitudinal Prospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


