Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3B: Luminal GI / Endoscopy / Pancreas
49 - Clinical Outcomes and Management of Gastric White Mucosal Patches in Patients With Familial Adenomatous Polyposis
Tuesday, October 28, 2025
2:45 PM - 2:55 PM PDT
Location: North Ballroom 120BC
- MA
Mohamad-Noor Abu-Hammour, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Mohamad-Noor Abu-Hammour, MD1, Natalie Farha, MD2, Amit Bhatt, MD3, Carol A.. Burke, MD, MACG1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic, Wichita, KS; 3Cleveland Clinic Foundation, Cleveland, OH
Introduction: Gastric white mucosal patches (WMPs) are endoscopic findings associated with a risk of gastric cancer (GC) in familial adenomatous polyposis (FAP). Optimal WMP management is unknown. We assessed resection modality, histology, and recurrence of WMP and any association with future advanced gastric pathology and GC.
Methods: FAP patients with WMPs ≥20 mm undergoing EGD at a single center from 2011-2025 were identified (Figure 1). Lesion characteristics, resection modality, histology, recurrence rates, and development of advanced gastric pathology were collected. Recurrence was defined as reappearance of WMP at the site of previous resection on serial EGD.
Results: Of 28 patients with a WMP, 18 underwent resection of 23 different WMPs with endoscopic mucosal resection (EMR, n=12), endoscopic submucosal dissection (ESD, n=5), hybrid ESD/EMR (n=4), and cold snare without submucosal lift (n=2). 3 patients with no resection follow-up were excluded. Of the remaining 15 patients, 18 WMPs were resected. Recurrence occurred in 100% (2/2) after cold snare without lift, 66.7% (6/9) after EMR, and 0% after ESD (0/4) or hybrid ESD/EMR (0/3) (Table 1). Mean post-resection surveillance follow-up was 50.3 mos (10.3-141.4 mos), with an average of 5.5 (3-14) follow-up EGDs/patient. WMP histology included gastric adenoma (GA) n=8; fundic gland polyp with low grade dysplasia (FGP-LGD) (n=5): intestinal type adenoma (n=2), FGP with high grade dysplasia (HGD) (n=1), FGP (n=1), and pylorid gland adenoma (PGA) with LGD (n=1). No patients undergoing endoscopic resection of WMP developed advanced gastric pathology on subsequent EGDs.
Of 10 patients without resection, 2 were excluded for no follow-up. In the 8 remaining patients, 3 developed GA with HGD or GC. Mean surveillance time was 59.1 mos (6.9-106.3 mos), with an average of 6.5 (2-14) follow-up EGDs/patient. Initial WMP histology was FGP-LGD (n=4), GA (n=2), PGA-LGD (n=1), and FGP (n=1).
Discussion: Over 1/3 of patients with unresected WMPs develop advanced gastric pathology within 5 years of detection, both within and outside the WMP. ESD and hybrid ESD/EMR are the optimal resection techniques for WMPs showing no recurrence or progression to advanced gastric pathology over 4 years. Understanding patient selection for resection, ensuring meticulous endoscopic surveillance, and using expert in endoscopic detection and resection of high-risk lesions are critical.
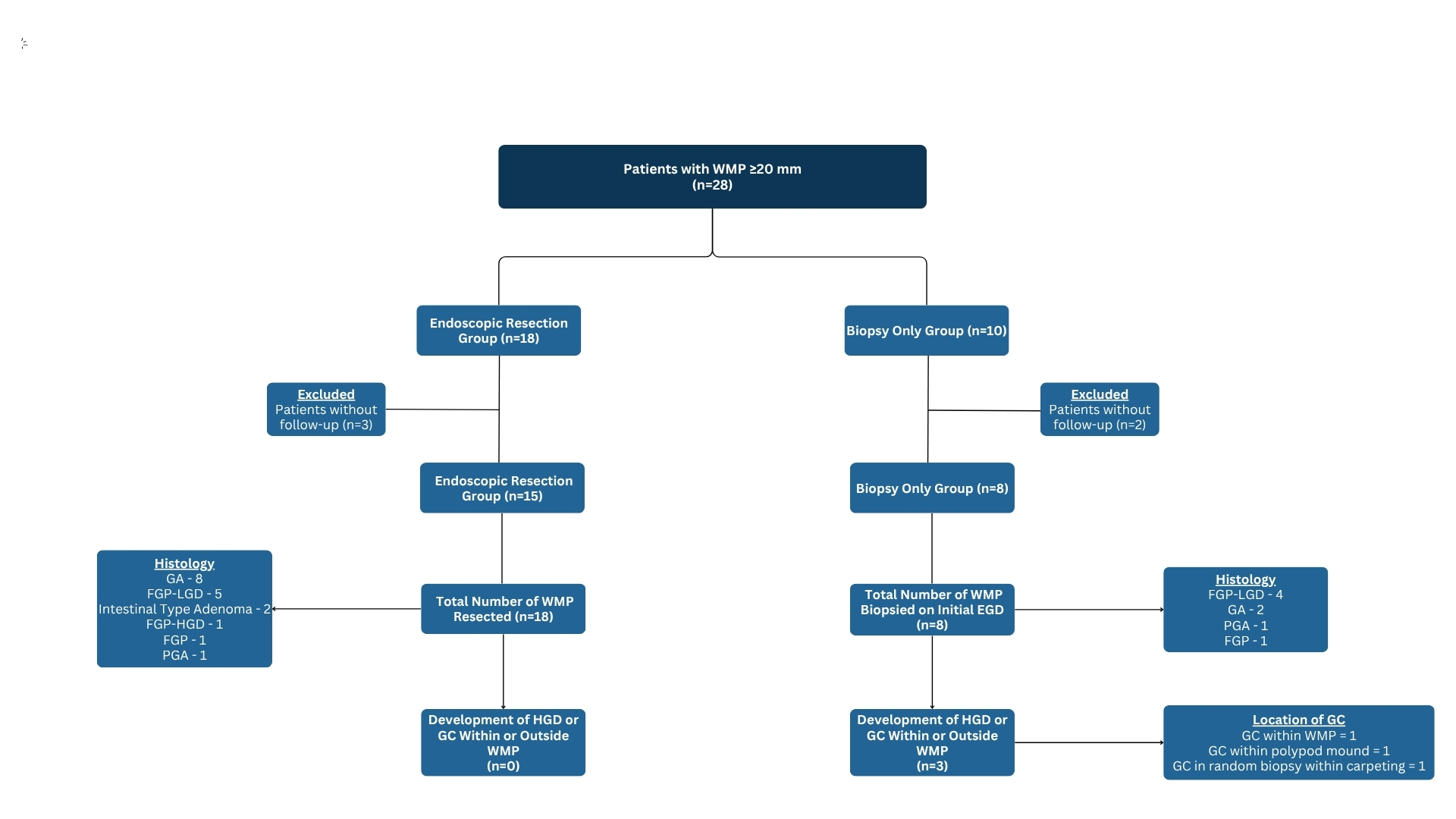
Figure: WMP, white mucosal patch; GA, gastric adenoma; FGP, fundic gland polyp; PGA, pyloric gland adenoma; TA, tubular adenoma; LGD, low-grade dysplasia; HGD, high-grade dysplasia; ND, no dysplasia

Figure: EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection; EGD, esophagogastroduodenoscopy; WMP, white mucosal patch; GA, gastric adenoma; FGP, fundic gland polyp; PGA, pyloric gland adenoma; TA, tubular adenoma; LGD, low-grade dysplasia; HGD, high-grade dysplasia; ND, no dysplasia
Disclosures:
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Natalie Farha indicated no relevant financial relationships.
Amit Bhatt indicated no relevant financial relationships.
Carol Burke: emtora biosciences – Grant/Research Support. lumabridge – Consultant. myriad – Food and beverage. Natera – Food and beverage.
Mohamad-Noor Abu-Hammour, MD1, Natalie Farha, MD2, Amit Bhatt, MD3, Carol A.. Burke, MD, MACG1, 49, Clinical Outcomes and Management of Gastric White Mucosal Patches in Patients With Familial Adenomatous Polyposis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic, Wichita, KS; 3Cleveland Clinic Foundation, Cleveland, OH
Introduction: Gastric white mucosal patches (WMPs) are endoscopic findings associated with a risk of gastric cancer (GC) in familial adenomatous polyposis (FAP). Optimal WMP management is unknown. We assessed resection modality, histology, and recurrence of WMP and any association with future advanced gastric pathology and GC.
Methods: FAP patients with WMPs ≥20 mm undergoing EGD at a single center from 2011-2025 were identified (Figure 1). Lesion characteristics, resection modality, histology, recurrence rates, and development of advanced gastric pathology were collected. Recurrence was defined as reappearance of WMP at the site of previous resection on serial EGD.
Results: Of 28 patients with a WMP, 18 underwent resection of 23 different WMPs with endoscopic mucosal resection (EMR, n=12), endoscopic submucosal dissection (ESD, n=5), hybrid ESD/EMR (n=4), and cold snare without submucosal lift (n=2). 3 patients with no resection follow-up were excluded. Of the remaining 15 patients, 18 WMPs were resected. Recurrence occurred in 100% (2/2) after cold snare without lift, 66.7% (6/9) after EMR, and 0% after ESD (0/4) or hybrid ESD/EMR (0/3) (Table 1). Mean post-resection surveillance follow-up was 50.3 mos (10.3-141.4 mos), with an average of 5.5 (3-14) follow-up EGDs/patient. WMP histology included gastric adenoma (GA) n=8; fundic gland polyp with low grade dysplasia (FGP-LGD) (n=5): intestinal type adenoma (n=2), FGP with high grade dysplasia (HGD) (n=1), FGP (n=1), and pylorid gland adenoma (PGA) with LGD (n=1). No patients undergoing endoscopic resection of WMP developed advanced gastric pathology on subsequent EGDs.
Of 10 patients without resection, 2 were excluded for no follow-up. In the 8 remaining patients, 3 developed GA with HGD or GC. Mean surveillance time was 59.1 mos (6.9-106.3 mos), with an average of 6.5 (2-14) follow-up EGDs/patient. Initial WMP histology was FGP-LGD (n=4), GA (n=2), PGA-LGD (n=1), and FGP (n=1).
Discussion: Over 1/3 of patients with unresected WMPs develop advanced gastric pathology within 5 years of detection, both within and outside the WMP. ESD and hybrid ESD/EMR are the optimal resection techniques for WMPs showing no recurrence or progression to advanced gastric pathology over 4 years. Understanding patient selection for resection, ensuring meticulous endoscopic surveillance, and using expert in endoscopic detection and resection of high-risk lesions are critical.
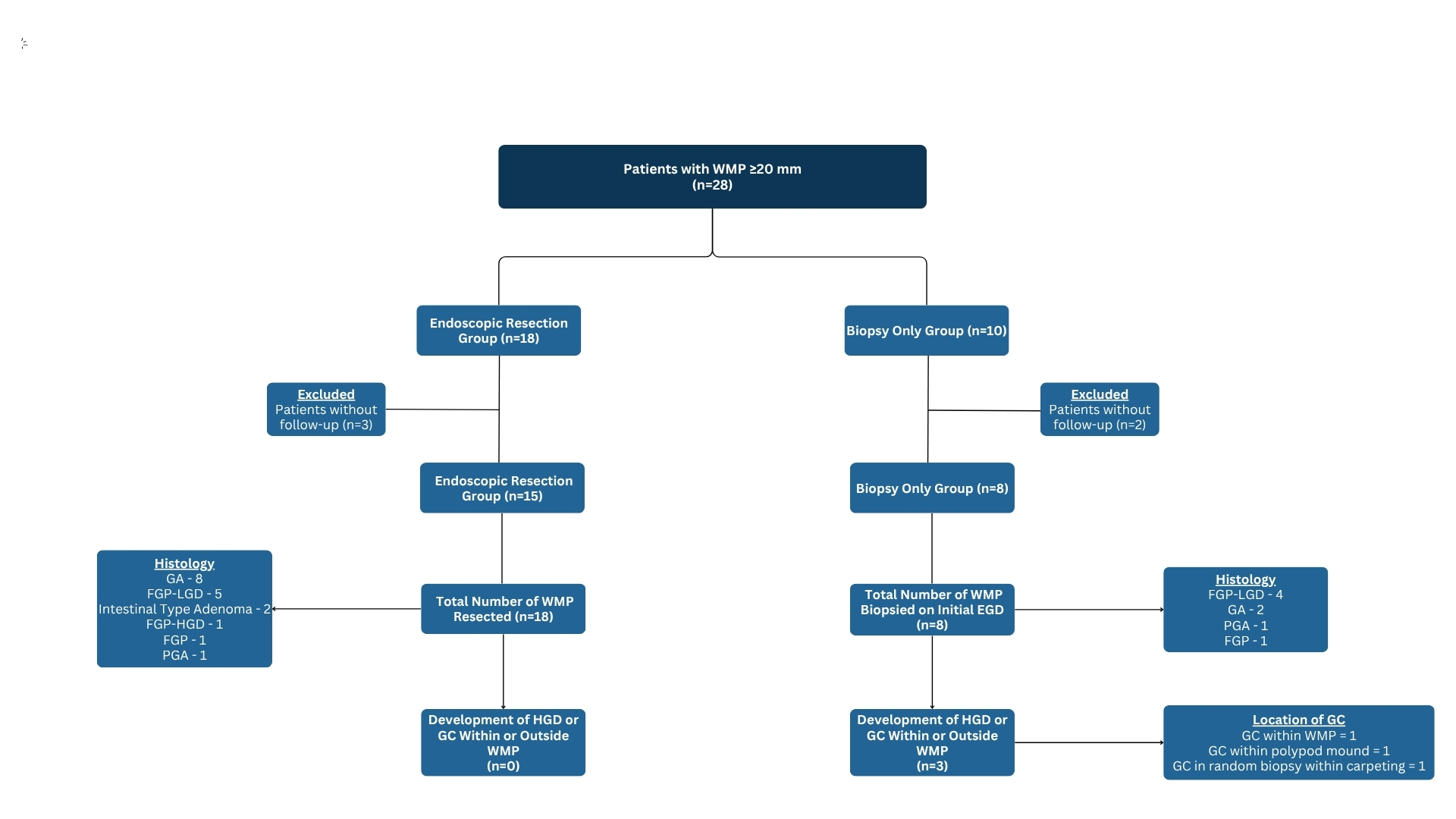
Figure: WMP, white mucosal patch; GA, gastric adenoma; FGP, fundic gland polyp; PGA, pyloric gland adenoma; TA, tubular adenoma; LGD, low-grade dysplasia; HGD, high-grade dysplasia; ND, no dysplasia

Figure: EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection; EGD, esophagogastroduodenoscopy; WMP, white mucosal patch; GA, gastric adenoma; FGP, fundic gland polyp; PGA, pyloric gland adenoma; TA, tubular adenoma; LGD, low-grade dysplasia; HGD, high-grade dysplasia; ND, no dysplasia
Disclosures:
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Natalie Farha indicated no relevant financial relationships.
Amit Bhatt indicated no relevant financial relationships.
Carol Burke: emtora biosciences – Grant/Research Support. lumabridge – Consultant. myriad – Food and beverage. Natera – Food and beverage.
Mohamad-Noor Abu-Hammour, MD1, Natalie Farha, MD2, Amit Bhatt, MD3, Carol A.. Burke, MD, MACG1, 49, Clinical Outcomes and Management of Gastric White Mucosal Patches in Patients With Familial Adenomatous Polyposis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

